|
Picture this.
You’re 50+, it has become difficult to keep your strength up like you could in your 30s and 40s. Your bone density is trending downwards, your ability to heal from fractures, sprains, surgeries and concussions is worse with each passing year..., and you suffer a fall. November is Falls Prevention Month. Click the following link which will take you to an article I wrote for Banff Sport Medicine, which offers numerous tips and tricks to help you and your love ones prevent life altering falls and injuries. https://banffsportmed.ca/preventing-slips-trips-and-falls/
0 Comments
New Role: Lead Physiotherapist It's been a busy last 6+ months of applying, interviewing, accepting a new role, and helping to establish a new clinic! I'm happy to announce my upcoming transition to work with an amazing team of orthopaedic surgeons, sport medicine physicians, physiotherapists and administrative staff. The newly constructed space at the Shops of Canmore will provide the footprint required to coordinate comprehensive, individualized, effective and collaborative treatment for all clients.
Since 2004, I've been involved in the health and fitness industry. Each step of my career progression has been marked by a desire to learn more, and create a positive impact on my clients and colleagues. In my new role I look forward to encouraging growth and collaboration amongst the physiotherapy team and the greater healthcare team of physicians and researchers. We are slated to start accepting Physiotherapy clients August 29, 2022. For more details, follow my Facebook page, Banff Sport Medicine Foundation's Facebook page or visit https://banffsportmed.ca/were-moving-and-expanding! #underoneroof Recovering from an injury can be a nuanced process - there are some symptoms that you should listen to and others that aren’t so important, poor information abounds during searches on Dr. Google, there are friendly recommendations to try certain products, drugs or stretches, and just when you think it is okay to resume your normal activities pain may re-surge. It can be confusing… That being said, if you focus your attention on the overarching principles of an effective rehab, recovery doesn’t have to be complicated! Here are few key areas that anyone can assess and will help to simply your return to wellness: 1. Time A) If you’ve sustained an injury, rehab will take time. Determining its severity can help you plan your rehab timeline. If it’s a small injury (micro-tearing or grade 1 sprain/strain), allow three days of relative rest for the injured area and slowly start to return to your sport. If it was a moderate or severe injury (grade 2-3 sprain / strain, fracture), you will need more time to allow the injury’s wound margins to heal back together. Due to the magnitude of a more severe injury you will likely benefit from a support (see below) and clever ways of modifying activity/programming. B) If you are not seeing many signs of improvement from your injury within a week, consulting a health care provider (Physio/Doctor) is a good idea. Diagnosing the injury and its severity will be important for your rehab strategy and long-term success. 2. Exercise A) Make sure that you perform exercises specific for your injury/dysfunction. Your exercises should address all three of the following:
3. Supports A) Your recovery from an injury may be uncomfortable but it needn’t be exquisitely painful. Utilizing walking aids (crutches/cane/walking poles), braces, taping techniques, medication (oral, topical or injections) or certain types of shoes/orthotics may help to alleviate some of your pain. These supports are not be relied on for very long, but can help reduce the harmful effects of feeling too much pain during your recovery. 4. Activity level A). Many of my clients see me because they have slow progress or are seeing no progress. This is often because #2 is not being addressed and clients are often doing too much or too little activity in their day to day life. Determining the appropriate amount of activity requires:
Concluding Remarks Creating a good rehab program is an art. Of course there are other items to consider whilst recovering from an injury, but if you can dial in these four key areas it should help with setting realistic expectations and executing a planned recovery.
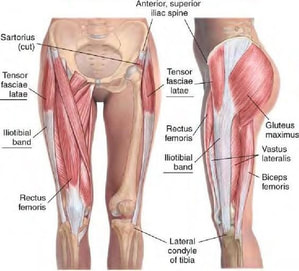
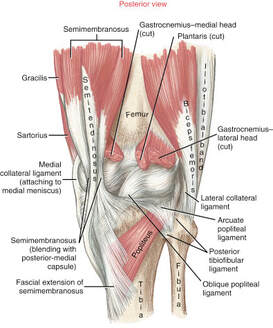
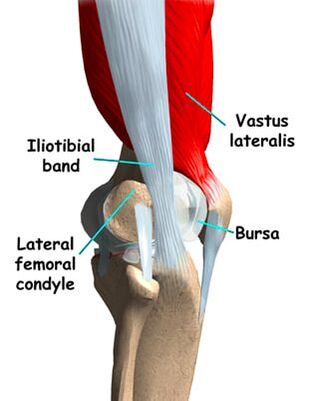
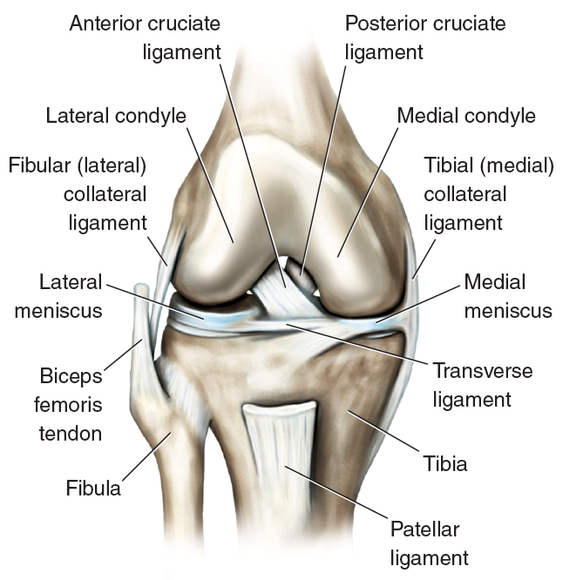
As always, if you have any questions feel free to send me an email or leave a comment! I was in Washington over the weekend cheering on a friend who was running the Orcas Island 50K - what a well run event! http://www.rainshadowrunning.com/orcas-island-50k.html After the race was finished, one of the runners discussed fear regarding pain on the outside of his knee. Paraphrasing, he said “I have IT band pain that started up around 20km and is quite sore now. It popped up in my last 50 mile race as well.” Despite finishing top 10, his next race will be his first 100 miler and has 3 times more elevation gain than the 50km race. His greatest fear was that his leg may have some bony protuberance that may cause persistent pain for the rest of his running career. This would be a legitimate concern if this were the case, but the truth is that this athlete jumped to these conclusions and hadn’t tried any strengthening exercises, mobility exercises or formal rehabilitation yet. It boggles my mind how a top 10 finisher can be so amazing at their sport yet but so blind to gaps in their training or rehab. Perhaps it is my cognitive bias, but I digress… haha Lateral Knee Pain Origin
Common Triggers in Developing Lateral Knee Pain Lateral knee pain due to the IT band or lateral quadriceps can arise for a number of reasons. Here are a few to consider: 1) Valgus (inward collapse of the knee) This may be caused by: - Reduced lateral hip muscle strength (often glute medius) - Compromised control of the hip muscles (how well the various hip muscles time contraction, intensity of contraction in response to various positions of the leg and in response to fatigue) - Structural or functional foot pronation… or shoes/orthotics that do not adequately support a neutral foot position 2) One leg that is shorter than the other Some people are born with or develop (usually through injury) a shorter leg. - The longer leg has to exert more effort to extend the knee in an effort to propulse the body forward - The shorter leg could be the victim as it must absorb more force with each landing step as the body will “drop” further down onto this leg with each step. 3) Running on a cambered surface - Always running on the left side of the road leads to running on a left leaning surface. It has the same impact as running on one leg that is shorter than the other. 4) Strength or mobility/flexibility imbalance - There is almost always a reason for side to side imbalances. It could be something you were born with or an old injury has led to a one-sided imbalance 5) Your tissues are not “load tolerant” enough to withstand all of the volume you ask of them - An increase of running volume too quickly in your program may not be tolerated - An increase of running intensity too quickly in your program may not be tolerated - Not enough load tolerance has been developed via strength training. Heavy squats, deadlifts, lunges, step ups and lateral hip strengthening exercises are a necessity. Concluding Remarks The first steps in finding a resolution requires an introspective analysis and physical assessment of the above items. If pathology exists at the tendon and a few weeks of local and regional treatment does not start to improve your pain then further evaluation may be helpful.
In my experience, when you are in pain it is always best to focus on movement quality and quantity. That is, are you doing the optimal amount and type of strengthening exercises and how is the quality of your movement? Are you doing the correct amount/type of running volume, and how is the quality of your running gait? Are you doing the optimal amount of mobility/flexibility work and is it actually helping to improve any of your limitations. Stay curious, fight to find answers and work hard! Impaired Tendon Stiffness Tendon stiffness is built up over months and years to match the loads we impose on our bodies. In the athletic realm, tendon stiffness increases via general strengthening and sport-specific training programs that either matches or is greater than the needs of our athletic pursuits. So you have tendon pain? We know that tendons with chronic pathology usually have changes in structure including thickening, increased extracellular fluid (also called ground substance) and degeneration of the collagen matrix. We also know that tendons with chronic pathology have reduced stiffness, which impairs the tendon’s ability to store and release energy as a healthy tendon would (1). So what factors can assist health care practitioners to determine who is more likely to develop tendon pathology? Also what strategies seem to work the best in improving tendon pain? I’ve extrapolated this blog post from a summary statement I wrote for Family Physicians in the Bow Valley. Read on and let me know if you have any questions or comments! Pathophysiology - Why do we develop tendon pain? Genetic Predisposition – Collagen diseases (Benign Hypermobility Syndrome, Ehler’s Danlos, Scleroderma) (2). Comorbidities that may predispose you to a greater risk of tendon pathology – Diabetes, thyroid, menstrual disorders, kidney disease, gallstones, gout (2,3). Environmental Overload – Change in activity, duration, intensity, footwear, sporting equipment, activity surface (2). Asymmetries –Biomechanical disadvantage secondary to stiff muscles, joints, poor strength, poor movement patterns/control (2). Solutions - Reducing pain and helping patients plan for long-term success. Step #1: Control Pre-Existing Medical Issues (from above). Step #2: Educate A) “You need to improve the strength of your tendon”. The best treatment outcomes occur from loading the tendon, improving movement patterns, building a proper training schedule, and reducing fears (4-7). B) “This may take a while”. Resolving irritable tendon pain can take months. Although it is a generalization, for every one month that your patient has had tendon pain, they can expect one month of strength and rehab work (4). C) “Some pain is acceptable during and after you exercise”. Ideally pain does not exceed 3/10 on a visual analogue scale, and symptoms should resolve quickly after exercise. Patients should perform a self-assessment 1 hour after exercise AND 24 hours later. If they experience increased levels of discomfort, they have loaded the tendon too much and must reassess their exercise form, and reduce the exercise volume or intensity (5). D) "Every tendon rehab is different". Each area of the body requires a different set of priorities and exercises to properly manage the tendon pathology. Your day-to-day activities, or athletic pursuits affect how you will heal and what is included in your rehab program. It is best to get a plan that is tailored for you. Step #3: UNLOAD The Tendon A) Physiotherapy: Reduce asymmetries in body. B) Reduce irritable activities but continue exercise. C) Tendon-specific unloading devices, if required. Step #4: Start To RELOAD The Tendon. Improve the tendon's ability to tolerate loads. A) Isometrics exercises involving the tendon, 2x/day. Perform 3 repetitions of 30 seconds hold and 30 seconds rest. Start with low intensity and increase as tolerated. Isometrics have been shown to reduce pain fairly quickly and is the necessary first step of loading the tendon before you can progress the patient to dynamic strengthening exercises (4,8-10). B) Dynamic strengthening exercises, 3x/week. 3-5 sets of 8 reps. Heavy and very slow (4,8-10). C) Activity/Sport Specific – Graduated return (4,8-10). Step #5: Consider Modalities And Injections. A) Extracorporeal Shockwave Therapy is a non-evasive technique that has a large and expanding amount of research to support its use in treating chronic tendinopathies (4,11). B) Injection therapies: If the aforementioned steps do not help to improve function consider referring the patient to a Sports Medicine Physician to determine any underlying pathology and possible cortisone injection, plasma-rich-protein injection, prolotherapy injection, or barbotage. Resolve There is almost always a way to escape tendon pain. Resolve to finding a health care team that understands tendon rehab, your sport, and fights as hard as you do to find answers. References 1) Arya S, Kulig K. Tendinopathy alters mechanical and material properties of the Achilles tendon. Journal of applied physiology. 2009 Nov 5;108(3):670-5.
2) Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology. 2006 Feb 20;45(5):508-21. 3) Ejnisman B, Andreoli CV, Monteiro GC, de Castro Pocchini A, Cohen C, Tortato S, Franklin MM, Machado AB, Cohen M. Calcifying tendinopathy: a local or a systemic condition?. Revista Brasileira de Ortopedia (English Edition). 2012 Jul 1;47(4):479-82. 3) Malliaras P, Cook J, Purdam C, Rio E. Patellar tendinopathy: clinical diagnosis, load management, and advice for challenging case presentations. journal of orthopaedic & sports physical therapy. 2015 Nov;45(11):887-98. 4) Smith BE, Hendrick P, Smith TO, Bateman M, Moffatt F, Rathleff MS, Selfe J, Logan P. Should exercises be painful in the management of chronic musculoskeletal pain? A systematic review and meta-analysis. Br J Sports Med. 2017 Dec 1;51(23):1679-87. 5) Kubo K, Ikebukuro T, Maki A, Yata H, Tsunoda N. Time course of changes in the human Achilles tendon properties and metabolism during training and detraining in vivo. Eur J Appl Physiol. 2012;112:2679–91. 6) Kubo K, Ikebukuro T, Yata H, Tsunoda N, Kanehisa H. Time course of changes in muscle and tendon properties during strength training and detraining. J Strength Cond Res. 2010;24:322–31. 7) de Boer MD, Maganaris CN, Seynnes OR, Rennie MJ, Narici MV. Time course of muscular, neural and tendinous adaptations to 23 day unilateral lower-limb suspension in young men. J Physiol. 2007;583:1079–91 8) Andres BM, Murrell GA. Treatment of tendinopathy: what works, what does not, and what is on the horizon. Clinical orthopaedics and related research. 2008. 1;466(7):1539-54. 9) Rio E, Kidgell D, Moseley GL, Gaida J, Docking S, Purdam C, Cook J. Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. Br J Sports Med. 2016 Feb 1;50(4):209-15. 10) Mani-Babu S, Morrissey D, Waugh C, Screen H, Barton C. The effectiveness of extracorporeal shock wave therapy in lower limb tendinopathy: a systematic review. The American journal of sports medicine. 2015 Mar;43(3):752-61. |
Have you found these article to be informative, helpful, or enjoyable to read? If so, please visit my Facebook page by clicking HERE, or click the Like button below to be alerted of all new articles!
Author
Jacob Carter lives and works in Canmore, Alberta. He combines research evidence with clinical expertise to educate other healthcare professionals, athletes, and the general public on a variety of health topics. Archives
November 2022
Categories
All
|
|
|











 RSS Feed
RSS Feed