|
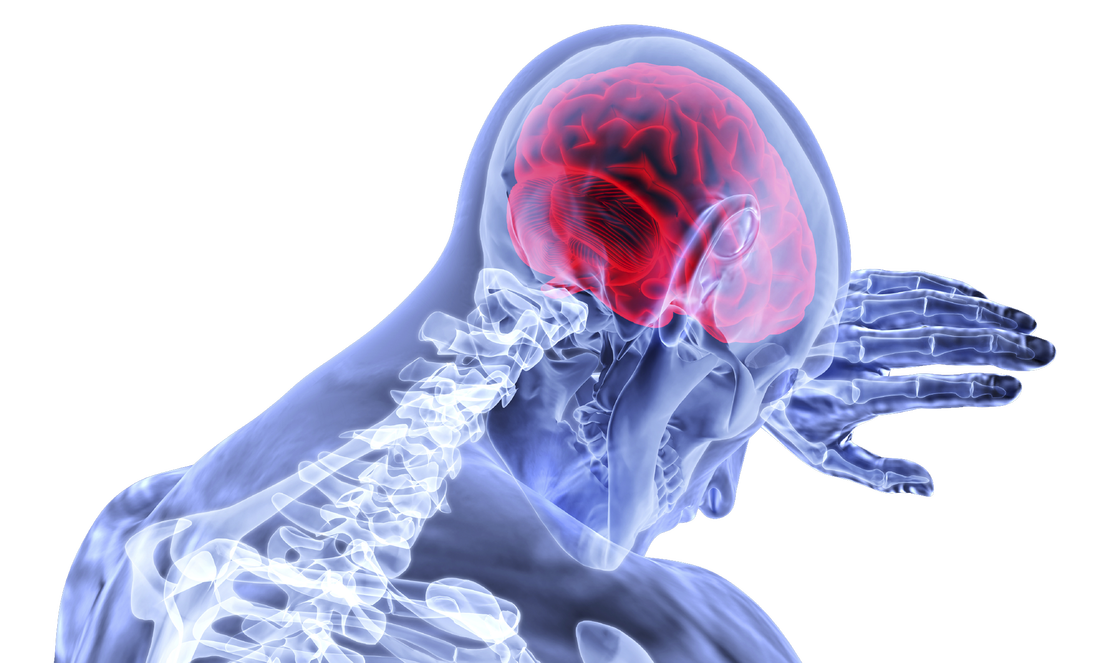
Although I've taken several courses that address concussion assessment and treatment over the last few years, research is continually advancing our knowledge of guidelines. Here is a summary I've put together of some of the most recent literature which aims to answer the questions: Which patients require concussion rehabilitation and what does recent evidence suggest that concussion rehabilitation should include? Assessment and Treatment Timelines The most recent International Consensus Statement on Concussion in Sport (The Berlin Consensus Statement, April 2017) states that evidence-based treatment for persistent concussion symptoms includes cervical spine treatment, vestibular rehabilitation, psychological interventions, and controlled submaximal exercise (1). The diagnosis of a concussion is a clinical judgment, made by a medical professional (1). A multi-faceted treatment approach seems to be the most effective approach to rehabilitation, and should begin immediately by obtaining a comprehensive history, performing a neurological exam to rule out serious pathology related to traumatic brain injury (TBI) or vascular insufficiency, and screening the cervical spine for signs of trauma. As a minimum, the health care team involved in the patient’s care should include a Family Physician and/or Sports Medicine Physician, and a Physiotherapist trained in concussion management. As required, patients may also benefit from a referral to see a psychologist, optometrist or dietician trained in concussion management. Recent evidence suggests that starting rehabilitation as early as 10 days after injury improves recovery time and decrease the risk of developing post-concussion syndrome (PCS) (2). For individuals with PCS, a multifaceted assessment is needed to identify targeted treatments that may be of benefit (3). Cervical, Vestibular, and Oculomotor Rehabilitation The amount of force necessary to sustain a concussion is far greater than that which is needed to sustain a whiplash (4). As a result, nearly every concussion sustains a whiplash as well. The significance of this fact is that whiplash injuries can disrupt the vestibular system (causing dizziness and vision dysfunction), result in cervical joint and muscle tightness/inflammation (causing local pain, referred headaches, and contribute to a lack of concentration), and disrupt the reflexes between cervical-vestibulo-occular system. In 2014, Schneider et al., published one of the first randomized clinical trials comparing a group receiving a combination of cervical and vestibular rehabilitation versus a control group that was given the usual protocol of rest followed by gradual exertion. Both groups received treatment from a physiotherapist at least once per week for 8 weeks, and had an average age of 15 years. In the treatment group, 73% of the participants were medically cleared within 8 weeks of initiation of treatment, compared with 7% in the control group. Individuals in the treatment group were 3.91 (95% CI 1.34 to 11.34) times more likely to be medically cleared by 8 weeks (2,5). In 2017, Reneker et al., published another randomized clinical trial comparing individualized treatment plans consisting of manual therapy of the neck, vestibular rehabilitation, oculomotor and neuromotor retraining, to a control group. Subjects were permitted by a sports medicine physician to enroll in the trial if they had experienced concussive symptoms for at least 10 days, and were treated by a Physiotherapist for up to a maximum of 8 visits or until they were fully cleared to return to play by a blinded sport-medicine physician. The progressive treatment group achieved symptom resolution and clearance to resume full sport activities significantly sooner than the control group: 15.5 days versus 26 days, respectively. The authors concluded that a personalized treatment plan beginning as early as 10 days after concussion may be an effective option to shorten recovery time (6). Exercise Recommendations Post-Concussion Initiating physical activity within the first 7-14 days post-concussion has been associated with a decreased risk of developing PCS. These results have been noted in adolescents and adults (7-12). Several clinical trial have demonstrated significant improvements in symptoms, cerebral blood flow mechanics, and complete return to all pre-injury activities over a much faster timeline compared to control groups or sham therapies (i.e. stretching). This is true for both acute concussions and PCS (7-10). Research would suggest performing low-level aerobic exercise most days of the week, at 80% of their symptom-tolerated heart rate (13,14). Summary: Providing Effective Treatment In addition to a graduated ‘Return to Learn’, ‘Return to Work’, and/or ‘Return to Play’ protocol, patients recovering from concussions seem to benefit the most from specific therapies for the cervical spine, vestibular system, visual system, and cardiovascular system. Research suggests that focused rehabilitation that begins within the first 7 to 10 days after injury can significantly improve outcomes and decrease long-term symptoms in both children and adults. References 1) McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, Cantu RC, Cassidy D, Echemendia RJ, Castellani RJ, Davis GA. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017 Apr 26:bjsports-2017.
2) Schneider K, Meeuwisse W, Nettel-Aguirre A, Boyd L, Barlow KM, Emery CA. Cervico-vestibular physiotherapy in the treatment of individuals with persistent symptoms following sport-related concussion: a randomized controlled trial. Br J Sports Med. 2014 May 1;48:1294-8. 3) Feddermann-Demont N, Echemendia RJ, Schneider KJ, Solomon GS, Hayden KA, Turner M, Dvořák J, Straumann D, Tarnutzer AA. What domains of clinical function should be assessed after sport-related concussion? A systematic review. Br J Sports Med. 2017 Jun 1;51(11):903-18. 4) Marshall CM, Vernon H, Leddy JJ, Baldwin BA. The role of the cervical spine in post-concussion syndrome. The Physician and sportsmedicine. 2015 Jul 3;43(3):274-84. 5) Schneider KJ, Meeuwisse WH, Barlow KM, Emery CA. Cervicovestibular rehabilitation following sport-related concussion. Br J Sports Med. 2018 Jan 1;52(2):100-1. 6) Reneker JC, Hassen A, Phillips RS, Moughiman MC, Donaldson M, Moughiman J. Feasibility of early physical therapy for dizziness after a sports‐related concussion: A randomized clinical trial. Scand J Med Sci Sports. 2017 Dec 1;27(12):2009-18. 7) Baker JG, Freitas MS, Leddy JJ, Kozlowski KF, Willer BS. Return to full functioning after graded exercise assessment and progressive exercise treatment of postconcussion syndrome. Rehab Res Pract. 2012. 8) Leddy JJ, Cox JL, Baker JG, Wack DS, Pendergast DR, Zivadinov R, Willer B. Exercise treatment for postconcussion syndrome: a pilot study of changes in functional magnetic resonance imaging activation, physiology, and symptoms. J Head Trauma Rehab. 2013 Jul 1;28(4):241-9. 9) Gagnon I, Grilli L, Friedman D, Iverson GL. A pilot study of active rehabilitation for adolescents who are slow to recover from sport- related concussion. Sci and J Med Sci Sports. 2015; 26(3):299–306. 10) Imhoff S, Fait P, Carrier-Toutant F, Boulard G. Efficiency of an active rehabilitation intervention in a slow-to-recover paediatric population following mild traumatic brain injury: a pilot study. J Sports Med. 2016. 11) Lal A, Kolakowsky-Hayner SA, Ghajar J, Balamane M. The Effect of Physical Exercise after a Concussion: A Systematic Review and Meta-Analysis. Am J Sports Med. 2017 Jun 1. 12) Zemek R, Grool AM, Aglipay M, Momoli F, Meehan WP, Freedman SB, Yeates KO, Gravel J, Gagnon I, Boutis K, Meeuwisse W. Relationship of early participation in physical activities to persistent post-concussive symptoms following acute paediatricpediatric concussion. Br J Sports Med. 2017 Jun 1;51(11):A20. 13] Schneider KJ, Leddy J, Guskiewicz K, Seifert TD, McCrea M, Silverberg N, Feddermann-Demont N, Iverson G, Hayden KA, Makdissi M: Rest and specific treatments following sport-related concussion: A systematic review. Br J Sports Med. 2017 Mar 24, 51:930-4. 14) Leddy JJ, Kozlowski K, Donnelly JP, Pendergast DR, Epstein LH, Willer B. A preliminary study of subsymptom threshold exercise training for refractory post-concussion syndrome. Clin J Sport Med. 2010 Jan 1;20(1):21-7
1 Comment
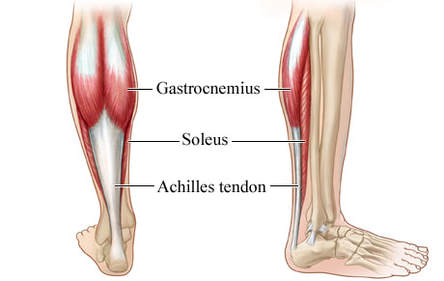
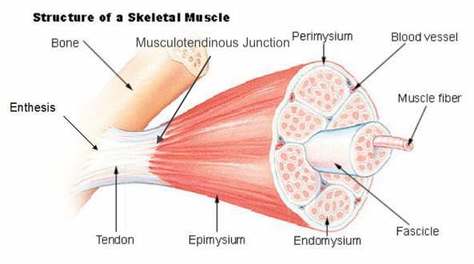
Basics of Tendon Function Tendons attach muscles to bones. Simple enough, right? Well... kind of... not really! Tendons are a specific type of force-transmitting architecture between a muscle and a bone. They are made of a strong fibrous collagen tissue and transmit the force of muscular contraction to a bone in an effort to create joint motion. Good quality tendons are like stiff springs; A stiff spring will stretch a little, and then recoil with most of the force that was required to stretch it initially. In our tendons, we call this stretch 'creep', and the recoil of the tissues 'recovery'. To prevent wasting energy and causing damage to a spring (or a tendon in this case), we need to have a certain degree of stiffness, resilience and efficiency. An example of this would be if I create tension in my calf by hopping on a single leg. The calf muscles transfer this fairly high load to my calcaneous bone via the achilles tendon. When I do this action repeatedly, a strong tendon will be able to handle the load that is asked of it... whereas a tendon with poor load tolerance may start to creep and not recover quickly... which means that some of the energy that was loaded into the tendon will be lost. This can lead to fatigue of the tissue, and eventually inflammation and micro or macrotearing of the tendon (small tears or a complete rupture). Peritendinous Dysfunction There are three common anatomical areas that lead to peritendinous dysfunction and pain: The weakest zones of a tendon are where it transitions from tendon to bone (enthesis), followed by the transition zone from muscle to tendon (musculotendinous junction) (1). Additionally, since tendons are mostly found near joints, they are protected from the hard bony surface by a bursa (a fluid-filled sac). If there is excessive compression of a tendon on a bursa, it will often become inflamed and irritable. This is more common than you'd expect, and often a diagnosed tendinopathy includes a bursitis. Creating Tendon Irritability Tendons become irritable when they are stressed beyond their load tolerance. Overuse may develop for one of many reasons: 1) Excessive volume: Tendons may not be able to adapt to an increased volume of a specific activity (over a period of days/weeks/months) 2) Poor biomechanics: Doing a motion differently than you may have done it previously (over a period of days/weeks/months) may cause irritability, even if the volume hasn't changed. If you've been doing a specific motion with poor biomechanics for a while, but then increase the volume, re-read principle #1. 3) Impaired mobility or strength elsewhere: Often, a proximal or distal impairment may cause you to (a) move poorly, which may ultimately cause you to over use some parts of your body and under-use others (b) compress on nerve tissues 4) Excessive stretching: Prolonged and frequent stretching of muscles/tendons may result in excessive creep and poor recovery of the tendon. Subsequent loading of the tendon may result in increased potential of tendon irritation. 5) Nerve compression: Decreased space at the intervertebral foramen (where the nerves exit your spine), or compression of a nerve by tight muscles may affect the strength of the muscles supplied by that nerve. This may cause poor movement patterns, referred pain, and /or dysfunctional muscle tone that may cause irritation of the tendon. 6) Maintenance required: Even with reasonable volume and good biomechanics, if you ask your body to perform an activity enough and don't ensure that the muscles maintain good mobility and tissue quality, the muscles may develop trigger points which in turn will pull on its tendon with increased tension. 7) Intrinsic factors: An individual's risk for developing tendinopathy is also affected by older age, sex, and systemic diseases such as Marfan's Syndrome, Ehlers–Danlos Syndrome, thyroid disorders, diabetes, rheumatoid arthritis, and having a predisposition to developing kidney stones, gallstones or gout(2). Changes on a Cellular Level Microtearing of tendon fibers will evoke a cascade of events, mainly in areas with poor blood supply: 1) Cytokines (small proteins that have an effect on the behavior of cells around them) activate tendon fibroblasts (cells that help to lay down type 3 collagen to help with the initial healing the cellular matrix that was disrupted). 2) At the same time, pain stimulating mechanisms are activated due to the inflammation that was created during the activity that damaged the tendon. 3) Other proteins in the area stimulate enzymes that degrade the extracellular matrix (the support network for tendon cells), and promotes the formation of new blood vasculature and new nerves (3). The result is a thicker, yet weaker tendon. It has a greater density of nerve endings which increases the sensitivity to all stimuli including the chronic inflammation. Together, these factors create a positive feedback system in which the inflammation irritates the nerve endings, causing increased inflammation... AND the chronic inflammation degrades the quality of the tendon itself. This means that when the tendon is loaded during sports or daily activities, further injury will occur to the tendon, thus creating additional inflammation and pain (3). 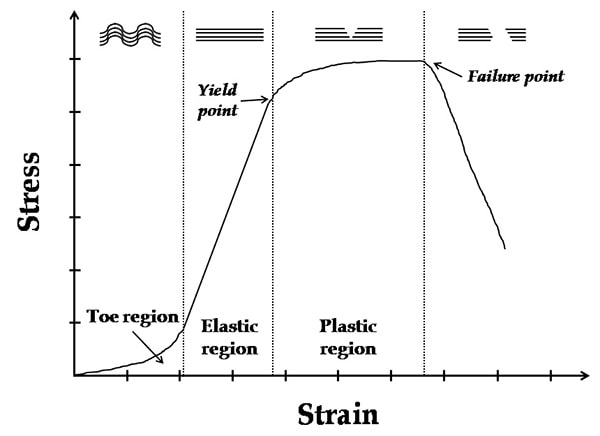 When a tendon is loaded or stretched beyond the elastic range, it experiences irreversible creep (plastic changes) to the tissue. This is known as microtearing, and will eventually lead to collagen / scar tissue formation, resulting in tendon thickening. If it continues beyond the plastic phase, macrofailure (a complete tear) of the tendon may occur (4,5). Tendon Take-Homes Statistically significant increases in tendon strength can be seen in the research after approximately 2-3 months of consistent strength training. Conversely, in a prolonged period of deloading, it only takes between 2-4 weeks to see statistically significant decreases in tendon strength (6-8). Therefore, a few general principles can be gleaned from all of the above information: 1) Train regularly, and do not take more than 2 weeks off from strength training, or else you may face the consequences. 2) Gradually increase your training volume in anything you do that is physically active. 3) Correct the mobility restrictions, strength impairments, and poor movement patterns that are within your control. Have a good personal trainer, coach, or physiotherapist assess your movement patterns. 4) If you are using your body regularly, use a foam roller regularly (poor man's massage therapist), and see a body worker (e.g. massage therapist or physiotherapist) for maintenance visits (once a month minimum). 5) Control your modifiable risk factors for developing comorbid conditions: Eat (mostly) healthy, sleep (mostly) well, and live a happy and stress-reduced life. Stay tuned for my next article that will examine elbow tendinopathy and management strategies! References 1) Apostolakos J, Durant TJ, Dwyer CR, Russell RP, Weinreb JH, Alaee F, Beitzel K, McCarthy MB, Cote MP, Mazzocca AD. The enthesis: a review of the tendon-to-bone insertion. Muscles, ligaments and tendons journal. 2014 Jul;4(3):333.
2) Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology. 2006 Feb 20;45(5):508-21. 3) Abate M, Silbernagel KG, Siljeholm C, Di Iorio A, De Amicis D, Salini V, Werner S, Paganelli R. Pathogenesis of tendinopathies: inflammation or degeneration?. Arthritis research & therapy. 2009 Jun;11(3):235. 4) Svensson RB, Hassenkam T, Hansen P, Magnusson SP. Viscoelastic behavior of discrete human collagen fibrils. Journal of the Mechanical Behavior of Biomedical Materials. 2010 Jan 1;3(1):112-5. 5) Ryan ED, Herda TJ, Costa PB, Walter AA, Hoge KM, Stout JR, Cramer JT. Viscoelastic creep in the human skeletal muscle–tendon unit. European journal of applied physiology. 2010 Jan 1;108(1):207-11. 6) Kubo K, Ikebukuro T, Maki A, Yata H, Tsunoda N. Time course of changes in the human Achilles tendon properties and metabolism during training and detraining in vivo. Eur J Appl Physiol. 2012;112:2679–91. 7) Kubo K, Ikebukuro T, Yata H, Tsunoda N, Kanehisa H. Time course of changes in muscle and tendon properties during strength training and detraining. J Strength Cond Res. 2010;24:322–31. 8) de Boer MD, Maganaris CN, Seynnes OR, Rennie MJ, Narici MV. Time course of muscular, neural and tendinous adaptations to 23 day unilateral lower-limb suspension in young men. J Physiol. 2007;583:1079–91 |
Have you found these article to be informative, helpful, or enjoyable to read? If so, please visit my Facebook page by clicking HERE, or click the Like button below to be alerted of all new articles!
Author
Jacob Carter lives and works in Canmore, Alberta. He combines research evidence with clinical expertise to educate other healthcare professionals, athletes, and the general public on a variety of health topics. Archives
November 2022
Categories
All
|
|
|




 RSS Feed
RSS Feed