|
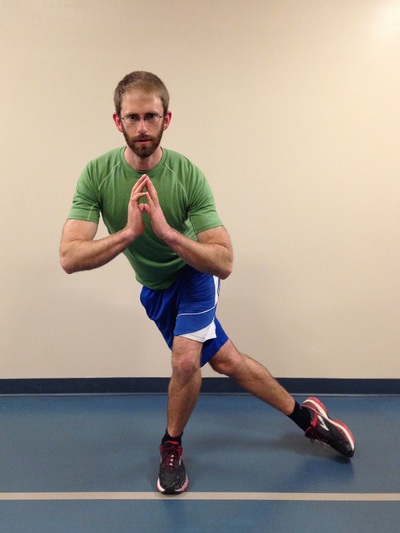
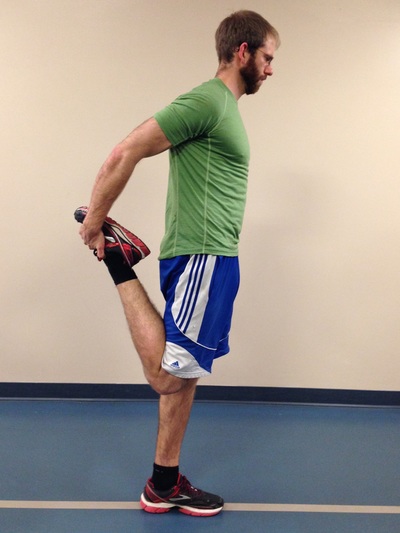
The Great Outdoors. It is there for you to enjoy, to push your limits, and develop fortitude. For some people, going outdoors can be synonymous with developing injuries, but there are steps you can take to mitigate future injuries from taking place. The Right Fitness Level Greater fitness leads to a better understanding of your limits, as well as the ability to achieve greater feats. A physical assessment by a good therapist or strength and conditioning coach can help you sort through the thousands of exercises out there to know which ones are relevant to your needs. - Slow, gradual increases in exercise and specific training are necessary (months and/or years). Our bodies adapt well to gradual stresses, but if too much load is placed on it at once, expect failure and injuries. It takes great dedication to yield great results. Most outdoor athletes peak in their 30s and 40s as they build cardiovascular endurance, muscular endurance, and a resistance to injury. - Outdoor athletes often suffer overuse / over-training. It is important to consider whether you have proper body mechanics during training and outdoor pursuits. Have knowledgeable therapists, coaches and other athletes watch your form and provide suggestions. It is also important to include adequate cross-training, regular body maintenance (physiotherapy, massage, rolling), proper nutrition, and adequate rest. - As a general rule there are certain joints which must be stable (strong ligamentous and muscular support around the joint, which prevents excess joint motion) and others which must have good mobility (the joint is built to be very flexible, however the muscular support around the joint must be able to control this increased range). As pertaining to lower body exercise, the core must be stable, hips must be mobile, knees must be stable, and the ankles must be mobile (Cook, Burton & Kiesel, 2010). Try adding the following 20-minute routine into your regular workouts, three days a week. It is a small corrective exercise program built to help the user become more aware of hip / knee / ankle positioning during single leg stance. It is not meant to replace regular strength training. Rather, it should enforce the principles of joint alignment, feeling posterior chain engagement and will allow good transfer to outdoor pursuits. A) Dynamic stretching. Perform dynamic stretching prior to exercise for 30 seconds per muscle group. A few lower body ideas include front/back and side-to-side leg swings, quick quadriceps stretches, quick piriformis/glute stretches, and hopping. B) Airplane. At first you may need to hold onto something for balance, but eventually you should be able to progress to no hands. Goal = 10 reps per side. C) Step-ups. Face a mirror and line up the hips and knees on the working leg to be approximately 90 degrees. Ensure that during the exercise, your knee tracks straight (not allowing it to collapse inwards or outwards). Lean forward, try to feel your glutes and hamstring fire on the upper leg then push through the heel on the working leg as you step up (this will help you to activate the posterior chain). Goal = 10 reps per side, with 2 times the expected weight of your backpack and gear. D) Single leg star balance. Reach as far in each of the four directions as possible, while bending the stance leg at the hip and knee during the reaching phase (this leg should remain straight in line from the hip to the foot). Goal = 10 reps for each leg. 1 rep = a full cycle of the four directions. Side note: Work to create symmetry in this test, as evidence suggests that a difference of more than 4 cm between left and right legs in ‘the forward reach’ component can help predict whether an athlete is at risk of injuring the leg (Smith, Chimera & Warren, 2014). Tip: Place masking tape on the ground and mark the distance in centimeters. E) Piriformis rolling and pigeon stretch. 1 minute rolling, 1 minute stretch per side. F) Lateral Quadriceps rolling and stretch. 1 minute rolling (focus on the outside of the leg), 1 minute stretch per side.
|
| Start With The Right Intel - Create specific training goals: How many days/hours, what gear do I need to use, am I familiar with the terrain? - Become efficient and effective in your skill-set by learning the best decision making skills and techniques via free resources (friends, books, videos), and progressing to courses or hiring a guide. | The Right Gear - Hiking poles take up to 25% of stress off your knees during descent (Schwameder, et al., 1999) help your legs save energy, and improve your balance on technical terrain. - Boots that fit well can prevent crushed toes, and rolled ankles. - Bring microspikes, mountaineering gear and/or avalanche gear if you expect snowy conditions. |
References
Schwameder, H., Roithner, R., Müller, E., Niessen ,W., Raschner, C. (1999).
Knee joint forces during downhill walking with hiking poles. Journal of Sports Science, 17(12): 969-978.
Smith, C.A., Chimera, N.J., Warren, M. (2014). Association of Y balance test reach asymmetry and injury in division I athletes. Medicine and Science in Sports and Exercise. Epub ahead of print.
Warning Signs
Some examples of objective signs may include changes (over the last week(s) / month(s) / year(s) in:
(1) Range of motion (ROM)
Has there been a change in your active or passive ROM? Does the end-feel of the last few degrees of your ROM feel the same as it always has? (i.e. does it feel like a muscle stretch, bone-on-bone, tissue approximation?
(2) Coordination
Can you perform simple and complex movement skills as easily as before? Are your movements performed with precision?
(3) Strength
Have you noticed any changes in your ability to access your muscle strength, endurance or power?
(4) Speed
Are you able to move as quickly in different movement patterns as before? Do you fatigue more easily?
(5) Symmetry
Are you able to control the left side of your body as well as you are on the right? Do your movements look symmetrical on both sides when you perform them in front of a mirror?
Some examples of subjective signs may include:
(1) Lack of confidence
Do you feel an incapability to execute the skill well? Does something just feel "off"? The skill may look well coordinated but may just feel uncoordinated.
(2) Poor decision-making when performing a skill
Are you able to make tactical decisions about using the skill? While performing a skill, are you able to make decisions regarding your environment to determine what your next course of action should be?
(3) Inability to multitask
Do you find it more difficult to talk (or do any number of other skill-sets) while you perform a skill?
(4) Poor body language
Do you feel awkward performing a skill that you used to be proficient in performing? Do other people seem to smile or chuckle while you perform the skill?
(5) Validated outcome measures
These outcome measures may help provide the patient with some insight into tasks they perform in their life that are difficult for them to do, even if they do not perceive symptoms to be present. This helps to create self-awareness. (Outcome measure examples include: Roland Morris Disability Questionnaire, Upper Extremity Functional Scale, Upper Extremity Functional Scale, etc.)
Onset of Symptoms
Your liberation from the symptoms will result from:
(1) Determining the root cause of the injury.
(2) Fixing the problem before permanent damage occurs.
(3) Learning from it and becoming more aware of your body.
(4) Developing more strength and coordination than before to prevent a similar injury from reoccurring.
(5) Gradual return to the sports / activities you enjoy.
Concluding Remarks
I’d like to start with the idea that ‘for human-beings, the expression of life is movement’. Another way to look at this idea would be to understand that movement is how all living-beings interact with their own environment. For example: #1) The small muscles that allow us to move our eyes, allow us to see the environment around us. #2) The muscles of our hand allow us to handle and manipulate objects, show affection, build a home, or a cook meal. Therefore, if you cannot move well, your physical, emotional, and mental health will suffer. The conclusion should be that being able to move well is in many ways like a medicine – it can create positive changes in our health.
The answer to better health (either primary, secondary or tertiary prevention of diseases/disorders) must be an interdisciplinary approach. Family Physicians, Optometrists, Dentists, and specialized health practitioners advise their patients that routine check-ups are preventative in nature, and may help to ensure optimal health. While their services may be essential, many health concerns still go unrecognized, unaddressed, untreated, or do not received adequate follow-up. The American Physical Therapy Association’s House of Delegates has a position statement on annual check-ups expressing “All individuals should visit a physical therapist at least annually to promote optimal health, wellness, and fitness, as well as to slow the progression of impairments, functional limitations, and disabilities”. While the Canadian Physiotherapy Association does not yet have a position statement on this matter they have agreed to bring the matter to the CEO’s attention who will relay the idea to the Board of Directors.
My opinion on the matter is this: (1) Physiotherapists have superior knowledge of anatomy, physical function and dysfunction, treating holistically, and also treating very specifically. (2) Physiotherapists develop more meaningful relationships with their patients than many other health professionals due to the additional time spent with their patients. This should allow for greater insight into current impairments and lead to a more timely physical diagnosis which can help correct current dysfunctions, decrease the negative effects of a current diagnosis, and/or prevent future dysfunction from occurring. (3) This means added time at a lower cost, which provides greater value for the patient: More time for assessment, treatment, and follow-up. (4) Physiotherapy has can reduce risk factors and/or treat the most common co-morbidities in Canada (e.g. heart disease, diabetes, obesity, chronic disease). (5) Patients can benefit from physiotherapy at any age in terms of development, health promotion and wellness, maintenance of health, and disease prevention. (6) Patients who are provided with consistent and competent medical attention decrease or delay future health problem severity, maintain their quality of life for longer, and decrease the future financial burden on the public healthcare system.
(1) This service is currently advertised by a minority of physiotherapists in Canada – The general public does not even know this is an option!
(2) Even if the general public had awareness, the expectations of the 21st century seem that if something is hard to achieve or attain, its not worth the initial effort.
(3) Only a minority of people in Canada have benefit coverage for physiotherapy, and private physiotherapy services cost money. How many people in Canada are actually willing to pay out-of-pocket to help themselves when they are not in acute pain? The funding needs to be driven provincially/federally, or through private insurance.
Suggestions for physiotherapists: Create a sample assessment of what should be included in an Annual Physiotherapy Assessment. Include a full body screen – put your neuro, cardioresp, AND MSK skills to use. Start advertising it and explain the benefits! Lobby your local physiotherapy association to increase interest in the matter!
Suggestions for other readers: Find a therapist that specializes in Annual Physiotherapy Assessments and preventative health. Get an assessment and live a healthier life! If you found your assessment helpful, spread the news to your significant others!
Author
Jacob Carter lives and works in Canmore, Alberta. He combines research evidence with clinical expertise to educate other healthcare professionals, athletes, and the general public on a variety of health topics.
Archives
November 2022
July 2022
January 2022
February 2020
May 2019
April 2019
July 2018
May 2018
March 2018
January 2018
October 2017
September 2017
March 2017
February 2017
December 2016
November 2016
October 2016
May 2016
March 2016
January 2016
June 2015
February 2015
December 2014
October 2014
September 2014
Categories
All
Aging Population
Annual Check Up
Annual Check-up
Annual Physiotherapy Assessment
Calgary
Canmore
Climbing
Collaborative Care
Concussion
Core Muscles
Disease Prevention
Exercise
Exercise Selection
FDN
Frozen Shoulder
Functional Dry Needling
Health
Health Promotion
IMS
Inflammation
Injuries
Injury Prevention
Intramuscular Stimulation
Jacob Carter
Literature Review
Lumbar Spine
Manual Therapy
Mountaineering
Pain
Personal Training
Physiotherapy
Preventative Medicine
Rehabilitation
Research
Shoulder Impingement
Shoulder Injuries
Skiing
Ski Injuries
Ski Season
Swelling
Tendinopathy
Tendinosis
Tendon
Tendonitis
Trail Running
Wellness
|
|















 RSS Feed
RSS Feed