|
Recovering from an injury can be a nuanced process - there are some symptoms that you should listen to and others that aren’t so important, poor information abounds during searches on Dr. Google, there are friendly recommendations to try certain products, drugs or stretches, and just when you think it is okay to resume your normal activities pain may re-surge. It can be confusing… That being said, if you focus your attention on the overarching principles of an effective rehab, recovery doesn’t have to be complicated! Here are few key areas that anyone can assess and will help to simply your return to wellness: 1. Time A) If you’ve sustained an injury, rehab will take time. Determining its severity can help you plan your rehab timeline. If it’s a small injury (micro-tearing or grade 1 sprain/strain), allow three days of relative rest for the injured area and slowly start to return to your sport. If it was a moderate or severe injury (grade 2-3 sprain / strain, fracture), you will need more time to allow the injury’s wound margins to heal back together. Due to the magnitude of a more severe injury you will likely benefit from a support (see below) and clever ways of modifying activity/programming. B) If you are not seeing many signs of improvement from your injury within a week, consulting a health care provider (Physio/Doctor) is a good idea. Diagnosing the injury and its severity will be important for your rehab strategy and long-term success. 2. Exercise A) Make sure that you perform exercises specific for your injury/dysfunction. Your exercises should address all three of the following:
3. Supports A) Your recovery from an injury may be uncomfortable but it needn’t be exquisitely painful. Utilizing walking aids (crutches/cane/walking poles), braces, taping techniques, medication (oral, topical or injections) or certain types of shoes/orthotics may help to alleviate some of your pain. These supports are not be relied on for very long, but can help reduce the harmful effects of feeling too much pain during your recovery. 4. Activity level A). Many of my clients see me because they have slow progress or are seeing no progress. This is often because #2 is not being addressed and clients are often doing too much or too little activity in their day to day life. Determining the appropriate amount of activity requires:
Concluding Remarks Creating a good rehab program is an art. Of course there are other items to consider whilst recovering from an injury, but if you can dial in these four key areas it should help with setting realistic expectations and executing a planned recovery.
As always, if you have any questions feel free to send me an email or leave a comment!
2 Comments
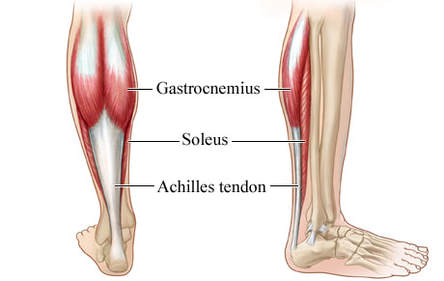
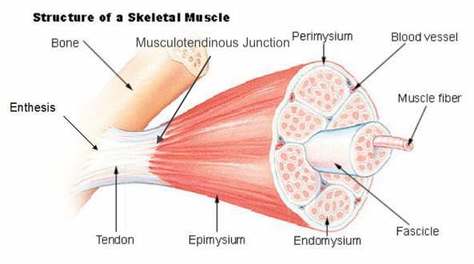
Basics of Tendon Function Tendons attach muscles to bones. Simple enough, right? Well... kind of... not really! Tendons are a specific type of force-transmitting architecture between a muscle and a bone. They are made of a strong fibrous collagen tissue and transmit the force of muscular contraction to a bone in an effort to create joint motion. Good quality tendons are like stiff springs; A stiff spring will stretch a little, and then recoil with most of the force that was required to stretch it initially. In our tendons, we call this stretch 'creep', and the recoil of the tissues 'recovery'. To prevent wasting energy and causing damage to a spring (or a tendon in this case), we need to have a certain degree of stiffness, resilience and efficiency. An example of this would be if I create tension in my calf by hopping on a single leg. The calf muscles transfer this fairly high load to my calcaneous bone via the achilles tendon. When I do this action repeatedly, a strong tendon will be able to handle the load that is asked of it... whereas a tendon with poor load tolerance may start to creep and not recover quickly... which means that some of the energy that was loaded into the tendon will be lost. This can lead to fatigue of the tissue, and eventually inflammation and micro or macrotearing of the tendon (small tears or a complete rupture). Peritendinous Dysfunction There are three common anatomical areas that lead to peritendinous dysfunction and pain: The weakest zones of a tendon are where it transitions from tendon to bone (enthesis), followed by the transition zone from muscle to tendon (musculotendinous junction) (1). Additionally, since tendons are mostly found near joints, they are protected from the hard bony surface by a bursa (a fluid-filled sac). If there is excessive compression of a tendon on a bursa, it will often become inflamed and irritable. This is more common than you'd expect, and often a diagnosed tendinopathy includes a bursitis. Creating Tendon Irritability Tendons become irritable when they are stressed beyond their load tolerance. Overuse may develop for one of many reasons: 1) Excessive volume: Tendons may not be able to adapt to an increased volume of a specific activity (over a period of days/weeks/months) 2) Poor biomechanics: Doing a motion differently than you may have done it previously (over a period of days/weeks/months) may cause irritability, even if the volume hasn't changed. If you've been doing a specific motion with poor biomechanics for a while, but then increase the volume, re-read principle #1. 3) Impaired mobility or strength elsewhere: Often, a proximal or distal impairment may cause you to (a) move poorly, which may ultimately cause you to over use some parts of your body and under-use others (b) compress on nerve tissues 4) Excessive stretching: Prolonged and frequent stretching of muscles/tendons may result in excessive creep and poor recovery of the tendon. Subsequent loading of the tendon may result in increased potential of tendon irritation. 5) Nerve compression: Decreased space at the intervertebral foramen (where the nerves exit your spine), or compression of a nerve by tight muscles may affect the strength of the muscles supplied by that nerve. This may cause poor movement patterns, referred pain, and /or dysfunctional muscle tone that may cause irritation of the tendon. 6) Maintenance required: Even with reasonable volume and good biomechanics, if you ask your body to perform an activity enough and don't ensure that the muscles maintain good mobility and tissue quality, the muscles may develop trigger points which in turn will pull on its tendon with increased tension. 7) Intrinsic factors: An individual's risk for developing tendinopathy is also affected by older age, sex, and systemic diseases such as Marfan's Syndrome, Ehlers–Danlos Syndrome, thyroid disorders, diabetes, rheumatoid arthritis, and having a predisposition to developing kidney stones, gallstones or gout(2). Changes on a Cellular Level Microtearing of tendon fibers will evoke a cascade of events, mainly in areas with poor blood supply: 1) Cytokines (small proteins that have an effect on the behavior of cells around them) activate tendon fibroblasts (cells that help to lay down type 3 collagen to help with the initial healing the cellular matrix that was disrupted). 2) At the same time, pain stimulating mechanisms are activated due to the inflammation that was created during the activity that damaged the tendon. 3) Other proteins in the area stimulate enzymes that degrade the extracellular matrix (the support network for tendon cells), and promotes the formation of new blood vasculature and new nerves (3). The result is a thicker, yet weaker tendon. It has a greater density of nerve endings which increases the sensitivity to all stimuli including the chronic inflammation. Together, these factors create a positive feedback system in which the inflammation irritates the nerve endings, causing increased inflammation... AND the chronic inflammation degrades the quality of the tendon itself. This means that when the tendon is loaded during sports or daily activities, further injury will occur to the tendon, thus creating additional inflammation and pain (3). 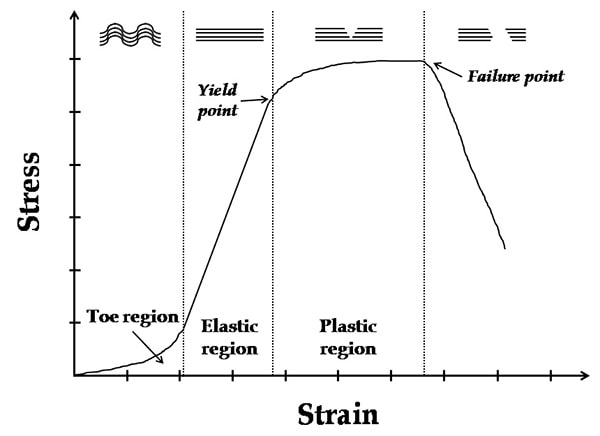 When a tendon is loaded or stretched beyond the elastic range, it experiences irreversible creep (plastic changes) to the tissue. This is known as microtearing, and will eventually lead to collagen / scar tissue formation, resulting in tendon thickening. If it continues beyond the plastic phase, macrofailure (a complete tear) of the tendon may occur (4,5). Tendon Take-Homes Statistically significant increases in tendon strength can be seen in the research after approximately 2-3 months of consistent strength training. Conversely, in a prolonged period of deloading, it only takes between 2-4 weeks to see statistically significant decreases in tendon strength (6-8). Therefore, a few general principles can be gleaned from all of the above information: 1) Train regularly, and do not take more than 2 weeks off from strength training, or else you may face the consequences. 2) Gradually increase your training volume in anything you do that is physically active. 3) Correct the mobility restrictions, strength impairments, and poor movement patterns that are within your control. Have a good personal trainer, coach, or physiotherapist assess your movement patterns. 4) If you are using your body regularly, use a foam roller regularly (poor man's massage therapist), and see a body worker (e.g. massage therapist or physiotherapist) for maintenance visits (once a month minimum). 5) Control your modifiable risk factors for developing comorbid conditions: Eat (mostly) healthy, sleep (mostly) well, and live a happy and stress-reduced life. Stay tuned for my next article that will examine elbow tendinopathy and management strategies! References 1) Apostolakos J, Durant TJ, Dwyer CR, Russell RP, Weinreb JH, Alaee F, Beitzel K, McCarthy MB, Cote MP, Mazzocca AD. The enthesis: a review of the tendon-to-bone insertion. Muscles, ligaments and tendons journal. 2014 Jul;4(3):333.
2) Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology. 2006 Feb 20;45(5):508-21. 3) Abate M, Silbernagel KG, Siljeholm C, Di Iorio A, De Amicis D, Salini V, Werner S, Paganelli R. Pathogenesis of tendinopathies: inflammation or degeneration?. Arthritis research & therapy. 2009 Jun;11(3):235. 4) Svensson RB, Hassenkam T, Hansen P, Magnusson SP. Viscoelastic behavior of discrete human collagen fibrils. Journal of the Mechanical Behavior of Biomedical Materials. 2010 Jan 1;3(1):112-5. 5) Ryan ED, Herda TJ, Costa PB, Walter AA, Hoge KM, Stout JR, Cramer JT. Viscoelastic creep in the human skeletal muscle–tendon unit. European journal of applied physiology. 2010 Jan 1;108(1):207-11. 6) Kubo K, Ikebukuro T, Maki A, Yata H, Tsunoda N. Time course of changes in the human Achilles tendon properties and metabolism during training and detraining in vivo. Eur J Appl Physiol. 2012;112:2679–91. 7) Kubo K, Ikebukuro T, Yata H, Tsunoda N, Kanehisa H. Time course of changes in muscle and tendon properties during strength training and detraining. J Strength Cond Res. 2010;24:322–31. 8) de Boer MD, Maganaris CN, Seynnes OR, Rennie MJ, Narici MV. Time course of muscular, neural and tendinous adaptations to 23 day unilateral lower-limb suspension in young men. J Physiol. 2007;583:1079–91 IntroductionThis article is meant to provide education to current clients, future clients, or any other interested parties. It will provide a basic level of knowledge which is available in the current research and should help to answer your question including: "How does it work?", and "Why does my muscle twitch when you put a needle there?!" Intramuscular Stimulation (IMS) is one of the most effective techniques available to reduce muscular pain and tightness; Essentially IMS 'resets' trigger points (TrPs) to allow for normal muscle contraction and relaxation. The technique is known by many names: IMS, GunnIMS, Dry Needling, Functional Dry Needling (FDN), Trigger Point Needling, and Intramuscular Manual Therapy. Regardless of the name, all methods use the same theory and should attain similar results, providing the diagnosis is correct and the practitioner is competent. The most recent systematic review, published in 2015, analyzed 25 high-quality studies and found significant improvement in pain, range of motion, function and quality of life when IMS was used in multiple body regions (1). Its reputation has become well-known: Many advocates from the medical and research community call IMS the most important contribution to pain science and treatment in the last 20 years. As a result it has become a highly sought after skill-set in professional sport, chronic pain centers and physiotherapy clinics everywhere. TrPs have been scientifically acknowledged since the early 1900s, when Sir William Gowers introduced the (now dated) term “fibrositis”, meaning a palpable tenderness and hardness of a muscle. Significant headway was made in the 1970s by Dr. Janet Travell (MD for Presidents Kennedy and Johnson) who authored research documenting TrP pain referral patterns. However, it wasn’t until Dr. Chan Gunn introduced his theories and supporting research in the late 1990s that IMS started to gain formal recognition as a treatment modality. Physiotherapists and physicians with specialized post-graduate training perform IMS. A thorough physical examination proves indispensable as chronic pain is neurologically driven (as opposed to structural), and therefore it is undetectable by X-rays, MRI Tests, Bone and CT Scans. If relevant TrPs are found on examination, a sterile acupuncture needle is then inserted and moved for 1-5 seconds in the tight muscle, causing a cramping or twitch response of the muscle. Needles may also be inserted near the spine where nerve roots have become irritated and hypersensitive. Before we can examine the effects of IMS on TrPs, let's first identify what we know about them. Three Types of Trigger Points There are three types of trigger points: Active Trigger Points – A hyperirritable spot in a taut band of skeletal muscle/fascia which is painful without being touched (but more painful with compression) and produces characteristic pain, referred symptoms, motor dysfunction and/or autonomic nervous system signs/symptoms. Latent Trigger Points – A hyperirritable spot that is painful with compression, but does not have referral symptoms. Satellite Trigger Points – A latent point that develops in a synergist muscle, antagonist muscle, muscle with common neural link or the same pain referral zone. These trigger points may become symptomatic neurogenically or mechanically by an increased irritability of the key TrP. Trigger Point Characteristics Trigger points have been studied thoroughly in the research. Here is what we know to date:
B) Elevated neurotransmitters and neuropeptides involved in pain sensitivity, vasoconstriction, vascular permeability, mast cell degranulation (mast cells release inflammatory components), increased sympathetic activity in motor endplate regions of TrP, decreased feedback control of muscle length and increased spontaneous electrical activity at motor endplates (14). C) Elevated cytokines and chemokines involved in inflammation, immune regulation, sensitivity of nociceptors and increased pain in the muscle (14). Physiological Effects of IMS As we insert an acupuncture needle into a TrP, a reset of the neuromuscular system occurs. This results in reduced local and referred pain (15, 16), improved range of motion (2, 3) and decreased TrP irritability both locally (7, 17) and remotely (8, 18). It is also proposed that these changes reduce associated dysfunction caused by the pulling effects of the tight muscles across joints, discs, nerves, tendons, etc. These results occur for the following reasons:
Conclusion IMS requires a medical examination and diagnosis by a practitioner knowledgeable in musculoskeletal pathology and human anatomy. The technique is supported by high-quality research, and when applied correctly, it can help provide lasting relief to patients with acute and chronic pain. References1) Boyles R, Fowler R, Ramsey D, Burrows E. Effectiveness of trigger point dry needling for multiple body regions: a systematic review. Journal of Manual and Manipulative Therapy. 2015 Jun 18:2042618615Y-0000000014.
2) Lucas KR, Rich PA, Polus BI. Muscle activation patterns in the scapular positioning muscles during loaded scapular plane elevation: the effects of latent myofascial trigger points. Clin Biomechanics. 2010;25(8):765-770. 3) Lucas KR, Polus BI, Rich PS. Latent myofascial trigger points: their effects on muscle activation and movement efficiency. J Bodyw Mov Ther. 2004;8:160-166. 4) Ballyns JJ, Shah JP, Hammond J, Gebreab T, Gerber LH, Sikdar S. Objective sonographic measures for characterizing myofascial trigger points associated with cervical pain. J Ultrasound Med. Oct 2011;30(10):1331-1340. 5) Brückle W, Sückfull M, Fleckenstein W, Weiss C, Müller W. Gewebe-pO2-Messung in der verspannten Rückenmuskulatur (m. erector spinae). Z. Rheumatol. 1990;49:208-216. 6) Ge HY, Fernandez-de-Las-Penas C, Yue SW. Myofascial trigger points: spontaneous electrical activity and its consequences for pain induction and propagation. Chin Med. 2011 Mar 25;6(13):1-7. 7) Kuan TS, Hsieh YL, Chen SM, Chen JT, Yen WC, Hong CZ. The myofascial trigger point region: correlation between the degree of irritability and the prevalence of endplate noise. Am J Phys Med Rehabil. 2007;86(3):183-189. 8) Hsieh YL, Chou LW, Joe YS, Hong CZ. Spinal cord mechanism involving the remote effects of dry needling on the irritability of myofascial trigger spots in rabbit skeletal muscle. Arch Phys Med Rehabil. Jul 2011;92(7): 1098-1105. 9) Rha DW, Shin JC, Kim YK, Jung JH, Kim YU, Lee SC. Detecting local twitch responses of myofascial trigger points in the lower-back muscles using ultrasonography. Archives of physical medicine and rehabilitation. 2011 Oct 31;92(10):1576-80. 10) Chen Q, Bensamoun S, Basford JR, Thompson JM, An KN. Identification and quantification of myofascial taut bands with magnetic resonance elastography. Archives of physical medicine and rehabilitation. 2007 Dec 31;88(12):1658-61. 11) Shah JP, Danoff JV, Desai MJ, et al. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil. Jan 2008;89(1):16-23. 12) Shah JP, Gilliams EA. Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: an application of muscle pain concepts to myofascial pain syndrome. J Bodyw Mov Ther. Oct 2008;12(4):371-384. 13) Shah J, Phillips T, Danoff JV, Gerber LH. A novel microanalytical technique for assaying soft tissue demonstrates significant quantitative biomechanical differences in 3 clinically distinct groups: normal, latent and active. Arch Phys Med Rehabil. 2003;84:A4. 14) Shah JP, Phillips TM, Danoff JV, Gerber LH. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. Journal of applied physiology. 2005 Nov 1;99(5):1977-84. 15) Affaitati G, Costantini R, Fabrizio A, Lapenna D, Tafuri E, Giamberardino MA. Effects of treatment of peripheral pain generators in fibromyalgia patients. Eur J Pain. Jan 2011;15(1): 61-69. 16) Srbely JZ, Dickey JP, Lee D, Lowerison M. Dry needle stimulation of myofascial trigger points evokes segmental anti-nociceptive effects. J Rehabil Med. 20110;42(5):463-468. 17) Chen JT, Chung KC, Hou CR, Kuan TS, Chen SM, Hong CZ. Inhibitory effect of dry needling on the spontaneous electrical activity recorded from myofascial trigger spots of rabbit skeletal muscle. Am J Phys Med Rehabil. Oct 2001;80(10):729-735. 18)Tsai C-T, Hsieh L-F, Kuan T-S, Kao M-J, Chou L-W, Hong C-Z. Remote effects of dry needling on the irritability of the myofascial trigger point in the upper trapezius muscle. Am J Phys Med Rehabil. 2010;89(2):133-140. 19) Cagnie B, Barbe T, De Ridder E, Van Oosterwijck J, Cools A, Danneels L. The influence of dry needling of the trapezius muscle on muscle blood flow and oxygenation. Journal of manipulative and physiological therapeutics. 2012 Dec 31;35(9):685-91. 20) Hsieh YL, Yang SA, Yang CC, Chou LW. Dry needling at myofascial trigger spots of rabbit skeletal muscles modulates the biochemicals associated with pain, inflammation, and hypoxia. Evidence-based complementary and alternative medicine. 2012 Dec 23;2012. 21) Niddam DM, Chan RC, Lee SH, Yeh TC, Hsieh JC. Central modulation of pain evoked from myofascial trigger point. The Clinical journal of pain. 2007 Jun 1;23(5):440-8. When it comes to exercising, there are a lot of choices to be made; How often do I work out? Which body parts should I exercise? How much cardio, core, stretching, etc.. etc.. should I do? How many sets/reps/minutes? The list goes on and on… I’m about to make the exercise selection part of your workout a bit easier. The following list describes 7 exercises that are best left OUT of your work out. Read and enjoy! If you have any comments or questions feel free to leave them in the comment section or contact me personally! 1) Behind The Head Lat Pull Down This is a great exercise to focus on mid and lower trap development as well as general lat development. You’ll see some of the strongest body builders in the gym doing it, and I only hope that they know it may be harming their neck and shoulders. Because of the head forward (neck protraction) position, you are likely to see muscles like the sternocleidomastoid (SCM), levator scapulae, and upper fibers of the trapezius (traps) tighten up. These muscles are common sources of neck pain, reducing functional neck range of motion, as well as encouraging scapular downward rotation, which can create or further exacerbate shoulder dysfunctions. Additionally, the position of extreme horizontal abduction and external rotation of the shoulder can cause a host of problems that are not limited to shoulder impingement syndrome, rotator cuff strains, labral irritation/tears, AC Joint compression, and ligamentous laxity. 2) Upright Row The upright row focuses on strengthening the middle and posterior delts, rhomboids and upper traps. It can certainly achieve this goal, however it comes with the risk of shoulder impingement. I personally do not recommend this exercise to many people, but if I do it is always with the limitation of not bringing the elbows up above the shoulder level (as seen in the above picture). 3) Traditional Sit-ups, Crunches and Machines that Simulate Sit-ups Stuart McGill would die and then roll over in his grave if I didn’t mention these exercises. Essentially, yes, these exercises can pack on some muscle and definition to the rectus abdominua, iliopsoas, rectus femoris, and the obliques… However to include these exercises in a regular exercise program is not worth the risk of injury. Going back to basics for a moment- the core is essentially meant to create spinal stability. Another way for me to say this is that the core musculature is meant to functionally operate as an anti-mover for the spine, contracting isometrically. When you do a sit-up you are concentrically contracting the anterior core muscles. Additionally, Stu McGill’s research shows that each intervertebral disc in the lumbar spine has a finite number of spine bends (flexion) that it can tolerate. Due to the structure of the discs, repeated flexion (think rounding the back) is one of the worst motions for lumbar spine health. Crunches, sit-ups, and most abdominal machines in the gym FLEX the spine! So ..stop it!.. and stick to planks, and other exercises that keep the back in a neutral stable position. 4) Leg Press I love the fact that you can really load up this machine and focus on leg strength, however there are three main flaws I see to using it: 1) The back and feet are planted and impacts the proper knee arthrokinematics (the movement of the joint surfaces) of the tibiofemoral joint to take place. Typically as you straighten the knee, there is a conjunction external rotation of the tibia on the femur. It is hypothesized that this machine will affect this conjunct movement. 2) The back is flexed and thus it experiences high levels of stress placed on the discs (especially at the lumbosacral junction). 3) The exercise does not have a lot of functional carry-over to sport or daily life – Have you ever known anyone to sit down and push 400 lbs of weight? My recommendation – Train functionally in an upright position! 5) Knee Extensions This machine is great for building quad mass, but is not great for the: 1) Patellofemoral Joint Arthrokinematics: (A) The way that the patella (knee cap) moves on the femoral condyles changes depending on whether you are performing an open or closed-chain exercise. Powers et al. (2003) found that the patellofemoral joint kinematics during non-weight-bearing (open chain) exercises could be characterized as the patella moving on the femur, while the kinematics during weight-bearing (closed chain) exercises could be characterized as the femur rotating underneath the stable. The latter of the two conditions provides the least amount of stress placed on the patellofemoral joint. (B) There is often additional stress placed on the patellofemoral joint because the load that you must push with your shin is anterior to the knee joint, whereas during a squat, the load is often through the knee joint or posterior to the knee joint. 2) Tibiofemoral Joint Arthrokinematics: For the same reason as explained in the leg press example above (#1), pushing your shin against the machine prevents some of the conjunct external rotation of the tibia on the femur, meaning that the joint mechanics may be dysfunctional and can lead to joint damage. 6) Back Extensions This may be a good exercise to put on some erector spinal bulk, but over facilitation of this muscle group is already a common occurrence. Classically this facilitation occurs because of poor spinal stability via inhibited/weak deep core muscles (most significant = the multifidus muscles in this scenario). Performing this exercise may result in increased facilitation of the already facilitated erector spinae muscles. 7) Almost All Seated Exercises Avoid almost all seated exercises, and especially ones that cause repeated lumbar rotation. The worst ones to avoid include exercises like the seated torso rotation machine, or any machines that force you into lumbar flexion (as mentioned above in #3). Remember Stuart McGills advice from above? The lumbar spine should be able to move dynamically, but have static stability when loaded. What i mean by this is that when the spine is not under any stress, we should have full range of motion through flexion, extension, rotation and side flexion. However, when loaded, the core muscles should provide stability and should remain static. If the spine moves when it is under load, additional shear and compression forces will occur, resulting in wear-and-tear on the spine. Lastly, when we must engage other muscle groups from a seated postion, we do not harness the stability and strength of the core. As a result we likely are weaker in that exercise, and we could be placing our body at risk for injury. Why? Because most sitting inhibits our ability to contract some of our core muscles (i.e. when sitting, the anterior abdominal cavity is compressed which inhibits the diaphragm from contracting), and some of our peri-core muscles (i.e. the glutes, hamstrings multifidi, erector spinae, etc. are lengthened and thus unable to contract as forcefully from the seated position). Concluding Remarks This is an interesting take on mobility that has helped me greatly: Always think about the body in terms of what should be mobile or stable. The following list will help to provide you with an understanding, and if applied correctly will help guide your training and any injury rehabilitation: Ankle — Mobile Knee — Stable Hip — Mobile Lumbar Spine — Stable Thoracic Spine — Mobile Scapula — Stable Glenohumeral — Mobile Remember that each joint should have full ROM regardless of its main purpose. Read more about this approach from Gray Cook’s book, 'Movement', ReferencesPowers, C.M., Ward, S.R., Fredericson, M., Guillet, M., Shellock, F.G. (2003). Patellofemoral kinematics during weight-bearing and non-weight-bearing knee extension in persons with lateral subluxation of the patella: a preliminary study. Journal of Orthopaedic and Sports Physical Therapy: 33(11): 677 – 685.
|
Have you found these article to be informative, helpful, or enjoyable to read? If so, please visit my Facebook page by clicking HERE, or click the Like button below to be alerted of all new articles!
Author
Jacob Carter lives and works in Canmore, Alberta. He combines research evidence with clinical expertise to educate other healthcare professionals, athletes, and the general public on a variety of health topics. Archives
November 2022
Categories
All
|
|
|














 RSS Feed
RSS Feed