|
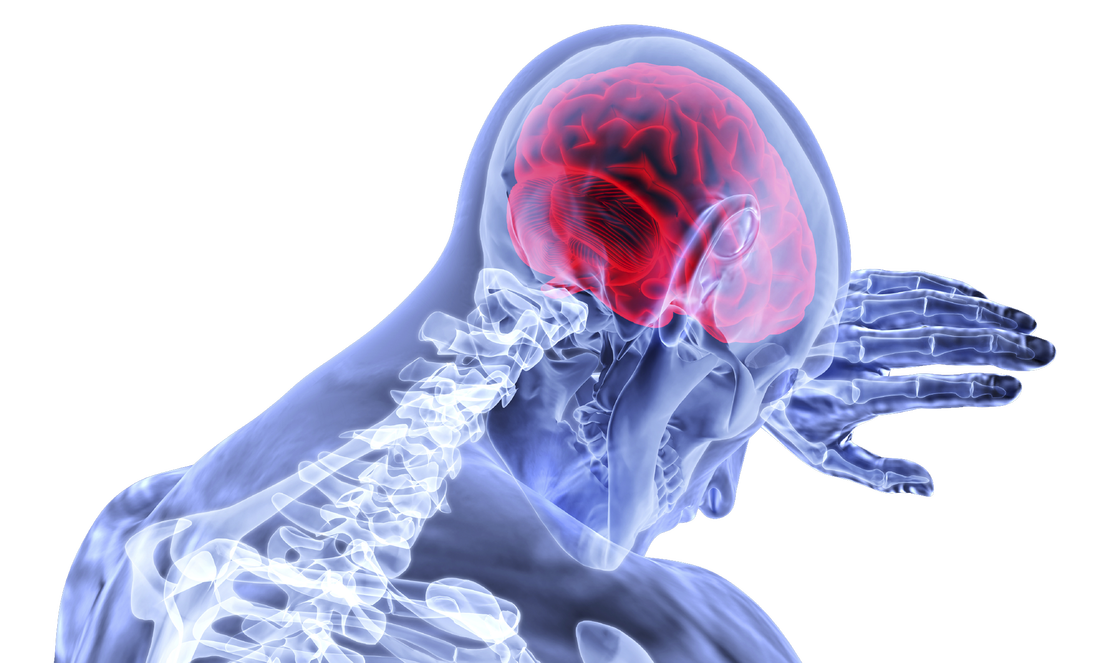
Although I've taken several courses that address concussion assessment and treatment over the last few years, research is continually advancing our knowledge of guidelines. Here is a summary I've put together of some of the most recent literature which aims to answer the questions: Which patients require concussion rehabilitation and what does recent evidence suggest that concussion rehabilitation should include? Assessment and Treatment Timelines The most recent International Consensus Statement on Concussion in Sport (The Berlin Consensus Statement, April 2017) states that evidence-based treatment for persistent concussion symptoms includes cervical spine treatment, vestibular rehabilitation, psychological interventions, and controlled submaximal exercise (1). The diagnosis of a concussion is a clinical judgment, made by a medical professional (1). A multi-faceted treatment approach seems to be the most effective approach to rehabilitation, and should begin immediately by obtaining a comprehensive history, performing a neurological exam to rule out serious pathology related to traumatic brain injury (TBI) or vascular insufficiency, and screening the cervical spine for signs of trauma. As a minimum, the health care team involved in the patient’s care should include a Family Physician and/or Sports Medicine Physician, and a Physiotherapist trained in concussion management. As required, patients may also benefit from a referral to see a psychologist, optometrist or dietician trained in concussion management. Recent evidence suggests that starting rehabilitation as early as 10 days after injury improves recovery time and decrease the risk of developing post-concussion syndrome (PCS) (2). For individuals with PCS, a multifaceted assessment is needed to identify targeted treatments that may be of benefit (3). Cervical, Vestibular, and Oculomotor Rehabilitation The amount of force necessary to sustain a concussion is far greater than that which is needed to sustain a whiplash (4). As a result, nearly every concussion sustains a whiplash as well. The significance of this fact is that whiplash injuries can disrupt the vestibular system (causing dizziness and vision dysfunction), result in cervical joint and muscle tightness/inflammation (causing local pain, referred headaches, and contribute to a lack of concentration), and disrupt the reflexes between cervical-vestibulo-occular system. In 2014, Schneider et al., published one of the first randomized clinical trials comparing a group receiving a combination of cervical and vestibular rehabilitation versus a control group that was given the usual protocol of rest followed by gradual exertion. Both groups received treatment from a physiotherapist at least once per week for 8 weeks, and had an average age of 15 years. In the treatment group, 73% of the participants were medically cleared within 8 weeks of initiation of treatment, compared with 7% in the control group. Individuals in the treatment group were 3.91 (95% CI 1.34 to 11.34) times more likely to be medically cleared by 8 weeks (2,5). In 2017, Reneker et al., published another randomized clinical trial comparing individualized treatment plans consisting of manual therapy of the neck, vestibular rehabilitation, oculomotor and neuromotor retraining, to a control group. Subjects were permitted by a sports medicine physician to enroll in the trial if they had experienced concussive symptoms for at least 10 days, and were treated by a Physiotherapist for up to a maximum of 8 visits or until they were fully cleared to return to play by a blinded sport-medicine physician. The progressive treatment group achieved symptom resolution and clearance to resume full sport activities significantly sooner than the control group: 15.5 days versus 26 days, respectively. The authors concluded that a personalized treatment plan beginning as early as 10 days after concussion may be an effective option to shorten recovery time (6). Exercise Recommendations Post-Concussion Initiating physical activity within the first 7-14 days post-concussion has been associated with a decreased risk of developing PCS. These results have been noted in adolescents and adults (7-12). Several clinical trial have demonstrated significant improvements in symptoms, cerebral blood flow mechanics, and complete return to all pre-injury activities over a much faster timeline compared to control groups or sham therapies (i.e. stretching). This is true for both acute concussions and PCS (7-10). Research would suggest performing low-level aerobic exercise most days of the week, at 80% of their symptom-tolerated heart rate (13,14). Summary: Providing Effective Treatment In addition to a graduated ‘Return to Learn’, ‘Return to Work’, and/or ‘Return to Play’ protocol, patients recovering from concussions seem to benefit the most from specific therapies for the cervical spine, vestibular system, visual system, and cardiovascular system. Research suggests that focused rehabilitation that begins within the first 7 to 10 days after injury can significantly improve outcomes and decrease long-term symptoms in both children and adults. References 1) McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, Cantu RC, Cassidy D, Echemendia RJ, Castellani RJ, Davis GA. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017 Apr 26:bjsports-2017.
2) Schneider K, Meeuwisse W, Nettel-Aguirre A, Boyd L, Barlow KM, Emery CA. Cervico-vestibular physiotherapy in the treatment of individuals with persistent symptoms following sport-related concussion: a randomized controlled trial. Br J Sports Med. 2014 May 1;48:1294-8. 3) Feddermann-Demont N, Echemendia RJ, Schneider KJ, Solomon GS, Hayden KA, Turner M, Dvořák J, Straumann D, Tarnutzer AA. What domains of clinical function should be assessed after sport-related concussion? A systematic review. Br J Sports Med. 2017 Jun 1;51(11):903-18. 4) Marshall CM, Vernon H, Leddy JJ, Baldwin BA. The role of the cervical spine in post-concussion syndrome. The Physician and sportsmedicine. 2015 Jul 3;43(3):274-84. 5) Schneider KJ, Meeuwisse WH, Barlow KM, Emery CA. Cervicovestibular rehabilitation following sport-related concussion. Br J Sports Med. 2018 Jan 1;52(2):100-1. 6) Reneker JC, Hassen A, Phillips RS, Moughiman MC, Donaldson M, Moughiman J. Feasibility of early physical therapy for dizziness after a sports‐related concussion: A randomized clinical trial. Scand J Med Sci Sports. 2017 Dec 1;27(12):2009-18. 7) Baker JG, Freitas MS, Leddy JJ, Kozlowski KF, Willer BS. Return to full functioning after graded exercise assessment and progressive exercise treatment of postconcussion syndrome. Rehab Res Pract. 2012. 8) Leddy JJ, Cox JL, Baker JG, Wack DS, Pendergast DR, Zivadinov R, Willer B. Exercise treatment for postconcussion syndrome: a pilot study of changes in functional magnetic resonance imaging activation, physiology, and symptoms. J Head Trauma Rehab. 2013 Jul 1;28(4):241-9. 9) Gagnon I, Grilli L, Friedman D, Iverson GL. A pilot study of active rehabilitation for adolescents who are slow to recover from sport- related concussion. Sci and J Med Sci Sports. 2015; 26(3):299–306. 10) Imhoff S, Fait P, Carrier-Toutant F, Boulard G. Efficiency of an active rehabilitation intervention in a slow-to-recover paediatric population following mild traumatic brain injury: a pilot study. J Sports Med. 2016. 11) Lal A, Kolakowsky-Hayner SA, Ghajar J, Balamane M. The Effect of Physical Exercise after a Concussion: A Systematic Review and Meta-Analysis. Am J Sports Med. 2017 Jun 1. 12) Zemek R, Grool AM, Aglipay M, Momoli F, Meehan WP, Freedman SB, Yeates KO, Gravel J, Gagnon I, Boutis K, Meeuwisse W. Relationship of early participation in physical activities to persistent post-concussive symptoms following acute paediatricpediatric concussion. Br J Sports Med. 2017 Jun 1;51(11):A20. 13] Schneider KJ, Leddy J, Guskiewicz K, Seifert TD, McCrea M, Silverberg N, Feddermann-Demont N, Iverson G, Hayden KA, Makdissi M: Rest and specific treatments following sport-related concussion: A systematic review. Br J Sports Med. 2017 Mar 24, 51:930-4. 14) Leddy JJ, Kozlowski K, Donnelly JP, Pendergast DR, Epstein LH, Willer B. A preliminary study of subsymptom threshold exercise training for refractory post-concussion syndrome. Clin J Sport Med. 2010 Jan 1;20(1):21-7
1 Comment
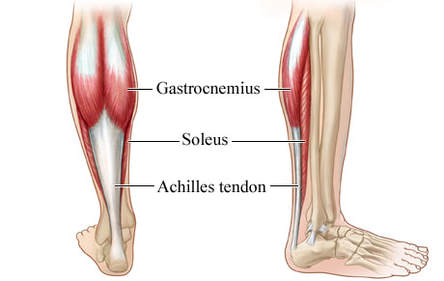
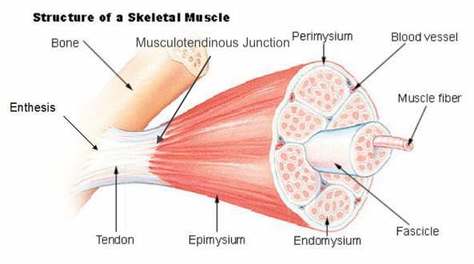
Basics of Tendon Function Tendons attach muscles to bones. Simple enough, right? Well... kind of... not really! Tendons are a specific type of force-transmitting architecture between a muscle and a bone. They are made of a strong fibrous collagen tissue and transmit the force of muscular contraction to a bone in an effort to create joint motion. Good quality tendons are like stiff springs; A stiff spring will stretch a little, and then recoil with most of the force that was required to stretch it initially. In our tendons, we call this stretch 'creep', and the recoil of the tissues 'recovery'. To prevent wasting energy and causing damage to a spring (or a tendon in this case), we need to have a certain degree of stiffness, resilience and efficiency. An example of this would be if I create tension in my calf by hopping on a single leg. The calf muscles transfer this fairly high load to my calcaneous bone via the achilles tendon. When I do this action repeatedly, a strong tendon will be able to handle the load that is asked of it... whereas a tendon with poor load tolerance may start to creep and not recover quickly... which means that some of the energy that was loaded into the tendon will be lost. This can lead to fatigue of the tissue, and eventually inflammation and micro or macrotearing of the tendon (small tears or a complete rupture). Peritendinous Dysfunction There are three common anatomical areas that lead to peritendinous dysfunction and pain: The weakest zones of a tendon are where it transitions from tendon to bone (enthesis), followed by the transition zone from muscle to tendon (musculotendinous junction) (1). Additionally, since tendons are mostly found near joints, they are protected from the hard bony surface by a bursa (a fluid-filled sac). If there is excessive compression of a tendon on a bursa, it will often become inflamed and irritable. This is more common than you'd expect, and often a diagnosed tendinopathy includes a bursitis. Creating Tendon Irritability Tendons become irritable when they are stressed beyond their load tolerance. Overuse may develop for one of many reasons: 1) Excessive volume: Tendons may not be able to adapt to an increased volume of a specific activity (over a period of days/weeks/months) 2) Poor biomechanics: Doing a motion differently than you may have done it previously (over a period of days/weeks/months) may cause irritability, even if the volume hasn't changed. If you've been doing a specific motion with poor biomechanics for a while, but then increase the volume, re-read principle #1. 3) Impaired mobility or strength elsewhere: Often, a proximal or distal impairment may cause you to (a) move poorly, which may ultimately cause you to over use some parts of your body and under-use others (b) compress on nerve tissues 4) Excessive stretching: Prolonged and frequent stretching of muscles/tendons may result in excessive creep and poor recovery of the tendon. Subsequent loading of the tendon may result in increased potential of tendon irritation. 5) Nerve compression: Decreased space at the intervertebral foramen (where the nerves exit your spine), or compression of a nerve by tight muscles may affect the strength of the muscles supplied by that nerve. This may cause poor movement patterns, referred pain, and /or dysfunctional muscle tone that may cause irritation of the tendon. 6) Maintenance required: Even with reasonable volume and good biomechanics, if you ask your body to perform an activity enough and don't ensure that the muscles maintain good mobility and tissue quality, the muscles may develop trigger points which in turn will pull on its tendon with increased tension. 7) Intrinsic factors: An individual's risk for developing tendinopathy is also affected by older age, sex, and systemic diseases such as Marfan's Syndrome, Ehlers–Danlos Syndrome, thyroid disorders, diabetes, rheumatoid arthritis, and having a predisposition to developing kidney stones, gallstones or gout(2). Changes on a Cellular Level Microtearing of tendon fibers will evoke a cascade of events, mainly in areas with poor blood supply: 1) Cytokines (small proteins that have an effect on the behavior of cells around them) activate tendon fibroblasts (cells that help to lay down type 3 collagen to help with the initial healing the cellular matrix that was disrupted). 2) At the same time, pain stimulating mechanisms are activated due to the inflammation that was created during the activity that damaged the tendon. 3) Other proteins in the area stimulate enzymes that degrade the extracellular matrix (the support network for tendon cells), and promotes the formation of new blood vasculature and new nerves (3). The result is a thicker, yet weaker tendon. It has a greater density of nerve endings which increases the sensitivity to all stimuli including the chronic inflammation. Together, these factors create a positive feedback system in which the inflammation irritates the nerve endings, causing increased inflammation... AND the chronic inflammation degrades the quality of the tendon itself. This means that when the tendon is loaded during sports or daily activities, further injury will occur to the tendon, thus creating additional inflammation and pain (3). 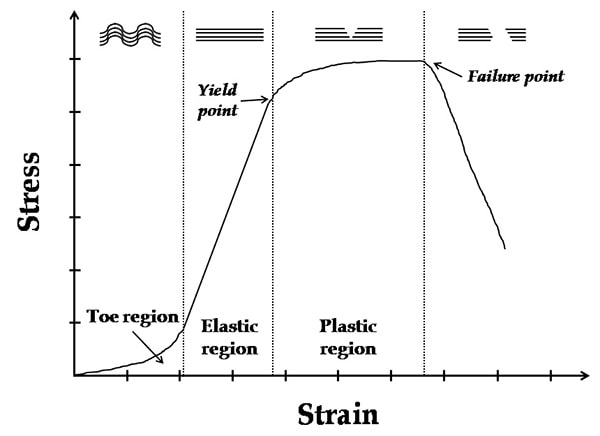 When a tendon is loaded or stretched beyond the elastic range, it experiences irreversible creep (plastic changes) to the tissue. This is known as microtearing, and will eventually lead to collagen / scar tissue formation, resulting in tendon thickening. If it continues beyond the plastic phase, macrofailure (a complete tear) of the tendon may occur (4,5). Tendon Take-Homes Statistically significant increases in tendon strength can be seen in the research after approximately 2-3 months of consistent strength training. Conversely, in a prolonged period of deloading, it only takes between 2-4 weeks to see statistically significant decreases in tendon strength (6-8). Therefore, a few general principles can be gleaned from all of the above information: 1) Train regularly, and do not take more than 2 weeks off from strength training, or else you may face the consequences. 2) Gradually increase your training volume in anything you do that is physically active. 3) Correct the mobility restrictions, strength impairments, and poor movement patterns that are within your control. Have a good personal trainer, coach, or physiotherapist assess your movement patterns. 4) If you are using your body regularly, use a foam roller regularly (poor man's massage therapist), and see a body worker (e.g. massage therapist or physiotherapist) for maintenance visits (once a month minimum). 5) Control your modifiable risk factors for developing comorbid conditions: Eat (mostly) healthy, sleep (mostly) well, and live a happy and stress-reduced life. Stay tuned for my next article that will examine elbow tendinopathy and management strategies! References 1) Apostolakos J, Durant TJ, Dwyer CR, Russell RP, Weinreb JH, Alaee F, Beitzel K, McCarthy MB, Cote MP, Mazzocca AD. The enthesis: a review of the tendon-to-bone insertion. Muscles, ligaments and tendons journal. 2014 Jul;4(3):333.
2) Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology. 2006 Feb 20;45(5):508-21. 3) Abate M, Silbernagel KG, Siljeholm C, Di Iorio A, De Amicis D, Salini V, Werner S, Paganelli R. Pathogenesis of tendinopathies: inflammation or degeneration?. Arthritis research & therapy. 2009 Jun;11(3):235. 4) Svensson RB, Hassenkam T, Hansen P, Magnusson SP. Viscoelastic behavior of discrete human collagen fibrils. Journal of the Mechanical Behavior of Biomedical Materials. 2010 Jan 1;3(1):112-5. 5) Ryan ED, Herda TJ, Costa PB, Walter AA, Hoge KM, Stout JR, Cramer JT. Viscoelastic creep in the human skeletal muscle–tendon unit. European journal of applied physiology. 2010 Jan 1;108(1):207-11. 6) Kubo K, Ikebukuro T, Maki A, Yata H, Tsunoda N. Time course of changes in the human Achilles tendon properties and metabolism during training and detraining in vivo. Eur J Appl Physiol. 2012;112:2679–91. 7) Kubo K, Ikebukuro T, Yata H, Tsunoda N, Kanehisa H. Time course of changes in muscle and tendon properties during strength training and detraining. J Strength Cond Res. 2010;24:322–31. 8) de Boer MD, Maganaris CN, Seynnes OR, Rennie MJ, Narici MV. Time course of muscular, neural and tendinous adaptations to 23 day unilateral lower-limb suspension in young men. J Physiol. 2007;583:1079–91 IntroductionThis article is meant to provide education to current clients, future clients, or any other interested parties. It will provide a basic level of knowledge which is available in the current research and should help to answer your question including: "How does it work?", and "Why does my muscle twitch when you put a needle there?!" Intramuscular Stimulation (IMS) is one of the most effective techniques available to reduce muscular pain and tightness; Essentially IMS 'resets' trigger points (TrPs) to allow for normal muscle contraction and relaxation. The technique is known by many names: IMS, GunnIMS, Dry Needling, Functional Dry Needling (FDN), Trigger Point Needling, and Intramuscular Manual Therapy. Regardless of the name, all methods use the same theory and should attain similar results, providing the diagnosis is correct and the practitioner is competent. The most recent systematic review, published in 2015, analyzed 25 high-quality studies and found significant improvement in pain, range of motion, function and quality of life when IMS was used in multiple body regions (1). Its reputation has become well-known: Many advocates from the medical and research community call IMS the most important contribution to pain science and treatment in the last 20 years. As a result it has become a highly sought after skill-set in professional sport, chronic pain centers and physiotherapy clinics everywhere. TrPs have been scientifically acknowledged since the early 1900s, when Sir William Gowers introduced the (now dated) term “fibrositis”, meaning a palpable tenderness and hardness of a muscle. Significant headway was made in the 1970s by Dr. Janet Travell (MD for Presidents Kennedy and Johnson) who authored research documenting TrP pain referral patterns. However, it wasn’t until Dr. Chan Gunn introduced his theories and supporting research in the late 1990s that IMS started to gain formal recognition as a treatment modality. Physiotherapists and physicians with specialized post-graduate training perform IMS. A thorough physical examination proves indispensable as chronic pain is neurologically driven (as opposed to structural), and therefore it is undetectable by X-rays, MRI Tests, Bone and CT Scans. If relevant TrPs are found on examination, a sterile acupuncture needle is then inserted and moved for 1-5 seconds in the tight muscle, causing a cramping or twitch response of the muscle. Needles may also be inserted near the spine where nerve roots have become irritated and hypersensitive. Before we can examine the effects of IMS on TrPs, let's first identify what we know about them. Three Types of Trigger Points There are three types of trigger points: Active Trigger Points – A hyperirritable spot in a taut band of skeletal muscle/fascia which is painful without being touched (but more painful with compression) and produces characteristic pain, referred symptoms, motor dysfunction and/or autonomic nervous system signs/symptoms. Latent Trigger Points – A hyperirritable spot that is painful with compression, but does not have referral symptoms. Satellite Trigger Points – A latent point that develops in a synergist muscle, antagonist muscle, muscle with common neural link or the same pain referral zone. These trigger points may become symptomatic neurogenically or mechanically by an increased irritability of the key TrP. Trigger Point Characteristics Trigger points have been studied thoroughly in the research. Here is what we know to date:
B) Elevated neurotransmitters and neuropeptides involved in pain sensitivity, vasoconstriction, vascular permeability, mast cell degranulation (mast cells release inflammatory components), increased sympathetic activity in motor endplate regions of TrP, decreased feedback control of muscle length and increased spontaneous electrical activity at motor endplates (14). C) Elevated cytokines and chemokines involved in inflammation, immune regulation, sensitivity of nociceptors and increased pain in the muscle (14). Physiological Effects of IMS As we insert an acupuncture needle into a TrP, a reset of the neuromuscular system occurs. This results in reduced local and referred pain (15, 16), improved range of motion (2, 3) and decreased TrP irritability both locally (7, 17) and remotely (8, 18). It is also proposed that these changes reduce associated dysfunction caused by the pulling effects of the tight muscles across joints, discs, nerves, tendons, etc. These results occur for the following reasons:
Conclusion IMS requires a medical examination and diagnosis by a practitioner knowledgeable in musculoskeletal pathology and human anatomy. The technique is supported by high-quality research, and when applied correctly, it can help provide lasting relief to patients with acute and chronic pain. References1) Boyles R, Fowler R, Ramsey D, Burrows E. Effectiveness of trigger point dry needling for multiple body regions: a systematic review. Journal of Manual and Manipulative Therapy. 2015 Jun 18:2042618615Y-0000000014.
2) Lucas KR, Rich PA, Polus BI. Muscle activation patterns in the scapular positioning muscles during loaded scapular plane elevation: the effects of latent myofascial trigger points. Clin Biomechanics. 2010;25(8):765-770. 3) Lucas KR, Polus BI, Rich PS. Latent myofascial trigger points: their effects on muscle activation and movement efficiency. J Bodyw Mov Ther. 2004;8:160-166. 4) Ballyns JJ, Shah JP, Hammond J, Gebreab T, Gerber LH, Sikdar S. Objective sonographic measures for characterizing myofascial trigger points associated with cervical pain. J Ultrasound Med. Oct 2011;30(10):1331-1340. 5) Brückle W, Sückfull M, Fleckenstein W, Weiss C, Müller W. Gewebe-pO2-Messung in der verspannten Rückenmuskulatur (m. erector spinae). Z. Rheumatol. 1990;49:208-216. 6) Ge HY, Fernandez-de-Las-Penas C, Yue SW. Myofascial trigger points: spontaneous electrical activity and its consequences for pain induction and propagation. Chin Med. 2011 Mar 25;6(13):1-7. 7) Kuan TS, Hsieh YL, Chen SM, Chen JT, Yen WC, Hong CZ. The myofascial trigger point region: correlation between the degree of irritability and the prevalence of endplate noise. Am J Phys Med Rehabil. 2007;86(3):183-189. 8) Hsieh YL, Chou LW, Joe YS, Hong CZ. Spinal cord mechanism involving the remote effects of dry needling on the irritability of myofascial trigger spots in rabbit skeletal muscle. Arch Phys Med Rehabil. Jul 2011;92(7): 1098-1105. 9) Rha DW, Shin JC, Kim YK, Jung JH, Kim YU, Lee SC. Detecting local twitch responses of myofascial trigger points in the lower-back muscles using ultrasonography. Archives of physical medicine and rehabilitation. 2011 Oct 31;92(10):1576-80. 10) Chen Q, Bensamoun S, Basford JR, Thompson JM, An KN. Identification and quantification of myofascial taut bands with magnetic resonance elastography. Archives of physical medicine and rehabilitation. 2007 Dec 31;88(12):1658-61. 11) Shah JP, Danoff JV, Desai MJ, et al. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil. Jan 2008;89(1):16-23. 12) Shah JP, Gilliams EA. Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: an application of muscle pain concepts to myofascial pain syndrome. J Bodyw Mov Ther. Oct 2008;12(4):371-384. 13) Shah J, Phillips T, Danoff JV, Gerber LH. A novel microanalytical technique for assaying soft tissue demonstrates significant quantitative biomechanical differences in 3 clinically distinct groups: normal, latent and active. Arch Phys Med Rehabil. 2003;84:A4. 14) Shah JP, Phillips TM, Danoff JV, Gerber LH. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. Journal of applied physiology. 2005 Nov 1;99(5):1977-84. 15) Affaitati G, Costantini R, Fabrizio A, Lapenna D, Tafuri E, Giamberardino MA. Effects of treatment of peripheral pain generators in fibromyalgia patients. Eur J Pain. Jan 2011;15(1): 61-69. 16) Srbely JZ, Dickey JP, Lee D, Lowerison M. Dry needle stimulation of myofascial trigger points evokes segmental anti-nociceptive effects. J Rehabil Med. 20110;42(5):463-468. 17) Chen JT, Chung KC, Hou CR, Kuan TS, Chen SM, Hong CZ. Inhibitory effect of dry needling on the spontaneous electrical activity recorded from myofascial trigger spots of rabbit skeletal muscle. Am J Phys Med Rehabil. Oct 2001;80(10):729-735. 18)Tsai C-T, Hsieh L-F, Kuan T-S, Kao M-J, Chou L-W, Hong C-Z. Remote effects of dry needling on the irritability of the myofascial trigger point in the upper trapezius muscle. Am J Phys Med Rehabil. 2010;89(2):133-140. 19) Cagnie B, Barbe T, De Ridder E, Van Oosterwijck J, Cools A, Danneels L. The influence of dry needling of the trapezius muscle on muscle blood flow and oxygenation. Journal of manipulative and physiological therapeutics. 2012 Dec 31;35(9):685-91. 20) Hsieh YL, Yang SA, Yang CC, Chou LW. Dry needling at myofascial trigger spots of rabbit skeletal muscles modulates the biochemicals associated with pain, inflammation, and hypoxia. Evidence-based complementary and alternative medicine. 2012 Dec 23;2012. 21) Niddam DM, Chan RC, Lee SH, Yeh TC, Hsieh JC. Central modulation of pain evoked from myofascial trigger point. The Clinical journal of pain. 2007 Jun 1;23(5):440-8. |
Have you found these article to be informative, helpful, or enjoyable to read? If so, please visit my Facebook page by clicking HERE, or click the Like button below to be alerted of all new articles!
Author
Jacob Carter lives and works in Canmore, Alberta. He combines research evidence with clinical expertise to educate other healthcare professionals, athletes, and the general public on a variety of health topics. Archives
November 2022
Categories
All
|
|
|




 RSS Feed
RSS Feed