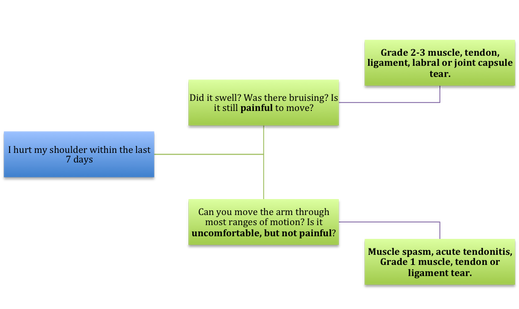
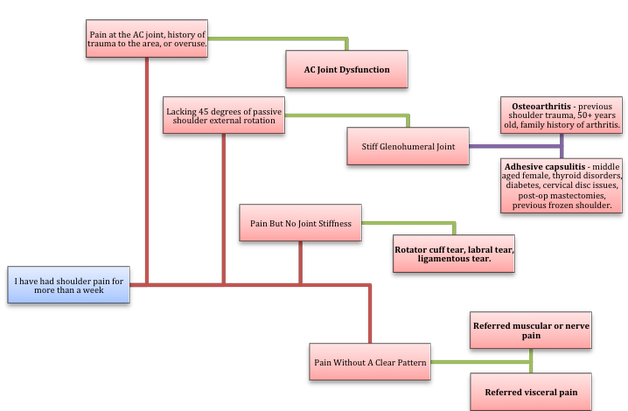
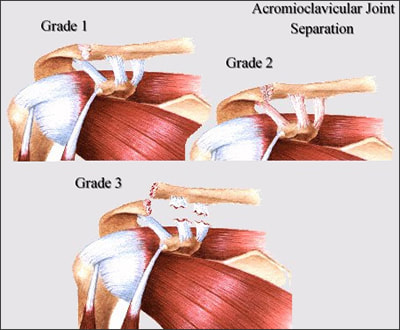
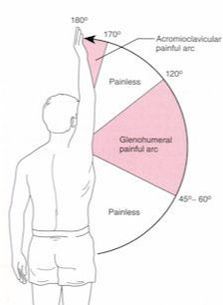
If Only Our Bodies Came With User Manuals! It's tough to know when its okay to push through pain or stiffness, or to know if the recent shoulder tweak that happened last week is of any importance. Over the last number of years I've picked up a number of strategies from research and experts in the sports medicine and orthopaedic world - I hope this can serve as a general guide! (NB - this is a blue print for simple shoulder injuries, and will not fit every situation. Use the following information as the guide that it is, and seek additional advice if you need further guidance!) Did You Hurt Your Shoulder Within The Last 7 Days? To start it off, if you've hurt your shoulder in the last 7 days, read through the following flow chart, and then the corresponding text below: Grade 2-3 muscle, tendon, ligament, labral or joint capsule tear If you experience significant pain, possibly with swelling or bruising, it is likely that you have significantly injured your soft tissues. While outliers exist (bone fracture or nerve involvement), it is most likely an issue related to a tear of a muscle, tendon, ligament, or the joint structure, If the pain in significant, a trip to the ER or family doctor may be the best first option. In terms of rehabilitation, it is probably best to let the shoulder heal for at least 7 days from the initial injury date before starting active rehab exercises. During this time you should see your local physiotherapist or sports medicine physician for an accurate diagnosis and to develop a treatment plan. During the first 7 days, you can support the shoulder with tape or a sling, apply ice (if you need to numb the pain), and perform pain-free range of motion. You should continue to exercise your lower body during this time. You can reasonably expect that there will be a range of motion limitation and/or strength reduction for at least 3 weeks from the date of the injury. It would be advisable to avoid loading the injured tissues with exercise for at least 3 weeks as the injury heals. As per standard tissue healing timelines, the injured tissues will not reach their full strength for up to 9-12 months in a healthy adult… so it is important that you do not re-injure it in the first 3-6 months (to be conservative). Muscle spasm, acute tendonitis, grade 1 muscle, tendon or ligament tear. If you've come to the conclusion that it's likely a muscle spasm, or minor muscle strain / ligament sprain, start immediately with soft tissue release, foam rolling, and gentle stretching into the areas of tightness. Within the first 3-7 days, start to do some light and pain-free resistance exercises to the surrounding muscles (e.g. easy rotator cuff exercises with a theraband). By the end of week 2 you should have loosened up most of the muscle tightness around the shoulder, and should be starting to gradually increase load/exercise for the shoulder. If your discomfort and limited range of motion is not gone within the first 2 weeks, get it assessed and treated. These small nagging injuries have a way of accumulating over the years and may predispose you to a more severe problem in the future. Have You Had Shoulder Pain For More Than 7 Days? This becomes more complicated as we have to discern between a number of different potential concerns. Acromioclavicular (AC) joint dysfunction - There are a few differed reasons that you may develop AC joint dysfunction. First, and most simple, is a direct hit to your shoulder. You will remember this happening, so in this case, its not too complicated. You will likely experience pain and joint laxity when you press on the AC joint, and in severe cases you may experience a 'separated shoulder' that looks like this: The good news about separated shoulders is that physiotherapy (as opposed to surgery) is often enough to help athletes and recreationalists return to their sports and daily activities pain free. If you do not remember a direct trauma, the following may apply to you: The AC joint is often the site of arthritis and come on from overuse or impact (most often seen in athletes (hockey, football, baseball, weight lifters, or overhead work). Pain and dysfunction from the AC joint often can cause impingement of the rotator cuff, and as such may present with muscle weakness, pain down the arm as far as the elbow, and a painful arc of motion. The symptoms that you experience during the arc of motion can help differentiate if it is just the joint that is irritable, or if there may be a rotator cuff impingement; If you have pain between 45-120 degrees abduction, but no pain before or after this range, then it is likely that you have an impingement of supraspinatus muscle (with or without an inflamed bursa). If you only have pain at the very top of this range of motion, it is likely that your AC joint is irritable. Assessment-informed treatment is often the key if it is a chronic pain: 1) You may benefit from other tests that can be done by a physiotherapist to assess joint integrity. 2) An X-ray may be of benefit to ensure there is no bone spur or congenital abnormality of the acromion, 3) A diagnostic ultrasound may be helpful to discern whether the supraspinatus tendon or subacromial bursa are irritated. Conservative treatment is the first-line treatment, as you will almost certainly have tightness and weakness of the surrounding shoulder musculature which may be causing secondary pain. A good assessment is usually needed to assess and treat the neck, thoracic spine, scapulothoracic rhythm, sternoclavicular joint mobility, scapulohumeral rhythm, and the AC joint. Most importantly, returning to a quality, pain-free exercise program will quicken the recovery. Differentiating Reasons for a Stiff Shoulder JointOne of the easiest ways to assess a stiff joint, is to look at passive range of motion, and try to assess the end-feel of the motion. If you are lacking 45 degrees of passive shoulder external rotation, and it feels like there is a capsular or joint restriction (hard end-feel), you likely fit into this category. Often, these cases require a medical approach to rule out other pathologies - be prepared to seek a referral to your family doctor or sports medicine physician for some imaging (to rule out sinister pathology or rule in arthritis), or blood work.  To assess passive shoulder external rotation, lay down on your back, and with you painful arm completely relaxed, use a broomstick or cane to gentle push the painful arm outwards (rotating the shoulder out). Keep your elbow relaxed and next to your ribcage. Remember... you are trying to assess the stiffness of the joint, so all muscles in the painful arm must remain relaxed! Glenohumeral Osteoarthritis If you have had a previous shoulder trauma, are 50+ years old or have a family history of arthritis, the most likely problem is that of glenohumeral osteoarthritis (could be from previous instability, or because of normal wear and tear associated with age). Manual therapy that focuses on improving joint capsule mobility is often required to make progress. Various joint injections exist that may help with lubrication of the joint, or inflammation within the joint. At home, patients can start with rolling tight muscles on the back of the shoulder joint to loosen any tissues that may be restricting the joint mobility. Ultimately, most progress will be made with the help of physiotherapy or medical intervention. Adhesive Capsulitis (Frozen Shoulder) The most likely alternative reason for a stiff shoulder is adhesive capsulitis. The strongest risk factor for developing adhesive capsulitis is being a peri-menopausal female. Other risk factors include thyroid disorders, diabetes, cervical disc issues, post-op mastectomies, a recent fall/trauma, and having a previous frozen shoulder. The shoulder seems to stiffen and become painful without a usual cause, and keeps patients awake at night. We see patterns of limited external rotation, internal rotation and flexion. If the diagnosis of adhesive capsulitis is reached, patients may find a cortisone injection helpful in the early stages. There has also been some clinical evidence showing that manipulation of the fibrotic joint under a nerve block may be of benefit.. Otherwise, regular physiotherapy that includes stretching, shockwave therapy, and manual therapy (soft tissue release, IMS, and joint mobilizations) will provide the greatest benefit. Shoulder Pain with Limited Active Range of Motion but Without Joint Stiffness If you do not have a stiff glenohumeral joint (more than 45 degrees passive external rotation), yet there is shoulder pain and limited active range of motion, a skilled practitioner will take you through a number of tests to help determine whether the pain is coming from a rotator cuff tear, labral tear or ligamentous tear (this is usually preceded by a dislocation / subluxation). The diagnosis of a tear must be ascertained by the clinic history, movement exam, special tests, response to treatment, and possibly ultrasound/MRI/other imaging. For the purposes of this article I am going to avoid the discussion of which special tests may be useful for diagnosing tears; This is a contentious issue as most special tests are... not that special; they are not very specific toward testing just one tissue and often lead to false positives. This topic is beyond the scope of this article. Shoulder Pain Without a Clear Pattern Very few patients fit into this category, so if you think that you do, its likely that you've missed something during your self-assessment. Excluding this caveat, I write this last section for completion. 1. Referred Pain - A painful shoulder that has no pattern of painful movement may be experiencing referred symptoms from the neck, diaphragm or the heart. 2. Cancer/Metastases - A number of different viscera can create pain into the shoulder region. Most likely include the lung, liver, and gallbladder. Typically you will experience unrelenting pain (nothing can make the symptoms change), difficulty sleeping at night, excessive fatigue, weight loss, a fever, or any number of other changes in your normal health. See the following link for more information: https://www.cancer.org/cancer/cancer-basics/signs-and-symptoms-of-cancer.html 3. Pain Syndromes - Widespread hypersensitivity/hyperalgesia may also affect the shoulder. Various non-specific pain syndromes may create shoulder pain and include: Chronic Regional Pain Syndrome, Myofascial Pain Syndrome & Fibromyalgia. A Final Note In most cases of shoulder pain, an exercise program is the key component necessary to return to full function without pain. In cases of partial thicken tendon tears, full thickness tendon tears or subacromial impingement, a specific and progressive exercise program often provides improved function, reduced pain and reduced need of surgery when compared with a general exercise program (1, 2, 3). My typical progression in the clinic is: 1) Determine if patient has any red flags that indicate immediate medical assessment / intervention. 2) Assess full body movement to determine how one area of the body may be affecting another. 3) Assess the shoulder for joint integrity, ligament and tendon damage, flexibility and strength. 4) Perform manual therapy, IMS and shockwave (if needed) to reduce pain and improve joint position/posture. 5) Provide patient with a specific, graduated exercise program. 6) Assess progress of the shoulder and repeat 2-6 as indicated until full function is .recovered, or a referral is indicated to see a sports medicine specialist. References (1) Björnsson Hallgren, H. C., Adolfsson, L. E., Johansson, K., Öberg, B., Peterson, A., & Holmgren, T. M. (2017). Specific exercises for subacromial pain: Good results maintained for 5 years. Acta Orthopaedica, 1-6.
(2) Holmgren, T., Hallgren, H. B., Öberg, B., Adolfsson, L., & Johansson, K. (2012). Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study. Bmj, 344, e787. (3) Kukkonen, J., Joukainen, A., Lehtinen, J., Mattila, K. T., Tuominen, E. K. J., Kauko, T., & Äärimaa, V. (2014). Treatment of non-traumatic rotator cuff tears. Bone Joint J, 96(1), 75-81.
0 Comments
When it comes to exercising, there are a lot of choices to be made; How often do I work out? Which body parts should I exercise? How much cardio, core, stretching, etc.. etc.. should I do? How many sets/reps/minutes? The list goes on and on… I’m about to make the exercise selection part of your workout a bit easier. The following list describes 7 exercises that are best left OUT of your work out. Read and enjoy! If you have any comments or questions feel free to leave them in the comment section or contact me personally! 1) Behind The Head Lat Pull Down This is a great exercise to focus on mid and lower trap development as well as general lat development. You’ll see some of the strongest body builders in the gym doing it, and I only hope that they know it may be harming their neck and shoulders. Because of the head forward (neck protraction) position, you are likely to see muscles like the sternocleidomastoid (SCM), levator scapulae, and upper fibers of the trapezius (traps) tighten up. These muscles are common sources of neck pain, reducing functional neck range of motion, as well as encouraging scapular downward rotation, which can create or further exacerbate shoulder dysfunctions. Additionally, the position of extreme horizontal abduction and external rotation of the shoulder can cause a host of problems that are not limited to shoulder impingement syndrome, rotator cuff strains, labral irritation/tears, AC Joint compression, and ligamentous laxity. 2) Upright Row The upright row focuses on strengthening the middle and posterior delts, rhomboids and upper traps. It can certainly achieve this goal, however it comes with the risk of shoulder impingement. I personally do not recommend this exercise to many people, but if I do it is always with the limitation of not bringing the elbows up above the shoulder level (as seen in the above picture). 3) Traditional Sit-ups, Crunches and Machines that Simulate Sit-ups Stuart McGill would die and then roll over in his grave if I didn’t mention these exercises. Essentially, yes, these exercises can pack on some muscle and definition to the rectus abdominua, iliopsoas, rectus femoris, and the obliques… However to include these exercises in a regular exercise program is not worth the risk of injury. Going back to basics for a moment- the core is essentially meant to create spinal stability. Another way for me to say this is that the core musculature is meant to functionally operate as an anti-mover for the spine, contracting isometrically. When you do a sit-up you are concentrically contracting the anterior core muscles. Additionally, Stu McGill’s research shows that each intervertebral disc in the lumbar spine has a finite number of spine bends (flexion) that it can tolerate. Due to the structure of the discs, repeated flexion (think rounding the back) is one of the worst motions for lumbar spine health. Crunches, sit-ups, and most abdominal machines in the gym FLEX the spine! So ..stop it!.. and stick to planks, and other exercises that keep the back in a neutral stable position. 4) Leg Press I love the fact that you can really load up this machine and focus on leg strength, however there are three main flaws I see to using it: 1) The back and feet are planted and impacts the proper knee arthrokinematics (the movement of the joint surfaces) of the tibiofemoral joint to take place. Typically as you straighten the knee, there is a conjunction external rotation of the tibia on the femur. It is hypothesized that this machine will affect this conjunct movement. 2) The back is flexed and thus it experiences high levels of stress placed on the discs (especially at the lumbosacral junction). 3) The exercise does not have a lot of functional carry-over to sport or daily life – Have you ever known anyone to sit down and push 400 lbs of weight? My recommendation – Train functionally in an upright position! 5) Knee Extensions This machine is great for building quad mass, but is not great for the: 1) Patellofemoral Joint Arthrokinematics: (A) The way that the patella (knee cap) moves on the femoral condyles changes depending on whether you are performing an open or closed-chain exercise. Powers et al. (2003) found that the patellofemoral joint kinematics during non-weight-bearing (open chain) exercises could be characterized as the patella moving on the femur, while the kinematics during weight-bearing (closed chain) exercises could be characterized as the femur rotating underneath the stable. The latter of the two conditions provides the least amount of stress placed on the patellofemoral joint. (B) There is often additional stress placed on the patellofemoral joint because the load that you must push with your shin is anterior to the knee joint, whereas during a squat, the load is often through the knee joint or posterior to the knee joint. 2) Tibiofemoral Joint Arthrokinematics: For the same reason as explained in the leg press example above (#1), pushing your shin against the machine prevents some of the conjunct external rotation of the tibia on the femur, meaning that the joint mechanics may be dysfunctional and can lead to joint damage. 6) Back Extensions This may be a good exercise to put on some erector spinal bulk, but over facilitation of this muscle group is already a common occurrence. Classically this facilitation occurs because of poor spinal stability via inhibited/weak deep core muscles (most significant = the multifidus muscles in this scenario). Performing this exercise may result in increased facilitation of the already facilitated erector spinae muscles. 7) Almost All Seated Exercises Avoid almost all seated exercises, and especially ones that cause repeated lumbar rotation. The worst ones to avoid include exercises like the seated torso rotation machine, or any machines that force you into lumbar flexion (as mentioned above in #3). Remember Stuart McGills advice from above? The lumbar spine should be able to move dynamically, but have static stability when loaded. What i mean by this is that when the spine is not under any stress, we should have full range of motion through flexion, extension, rotation and side flexion. However, when loaded, the core muscles should provide stability and should remain static. If the spine moves when it is under load, additional shear and compression forces will occur, resulting in wear-and-tear on the spine. Lastly, when we must engage other muscle groups from a seated postion, we do not harness the stability and strength of the core. As a result we likely are weaker in that exercise, and we could be placing our body at risk for injury. Why? Because most sitting inhibits our ability to contract some of our core muscles (i.e. when sitting, the anterior abdominal cavity is compressed which inhibits the diaphragm from contracting), and some of our peri-core muscles (i.e. the glutes, hamstrings multifidi, erector spinae, etc. are lengthened and thus unable to contract as forcefully from the seated position). Concluding Remarks This is an interesting take on mobility that has helped me greatly: Always think about the body in terms of what should be mobile or stable. The following list will help to provide you with an understanding, and if applied correctly will help guide your training and any injury rehabilitation: Ankle — Mobile Knee — Stable Hip — Mobile Lumbar Spine — Stable Thoracic Spine — Mobile Scapula — Stable Glenohumeral — Mobile Remember that each joint should have full ROM regardless of its main purpose. Read more about this approach from Gray Cook’s book, 'Movement', ReferencesPowers, C.M., Ward, S.R., Fredericson, M., Guillet, M., Shellock, F.G. (2003). Patellofemoral kinematics during weight-bearing and non-weight-bearing knee extension in persons with lateral subluxation of the patella: a preliminary study. Journal of Orthopaedic and Sports Physical Therapy: 33(11): 677 – 685.
|
Have you found these article to be informative, helpful, or enjoyable to read? If so, please visit my Facebook page by clicking HERE, or click the Like button below to be alerted of all new articles!
Author
Jacob Carter lives and works in Canmore, Alberta. He combines research evidence with clinical expertise to educate other healthcare professionals, athletes, and the general public on a variety of health topics. Archives
November 2022
Categories
All
|
|
|










 RSS Feed
RSS Feed