History of Knee Pain It's about this time of year, every year, that people living in north of California think about strapping on skis for the winter. The most common concern is regarding knee integrity and readiness to ski. I like to group the concern into three groups:
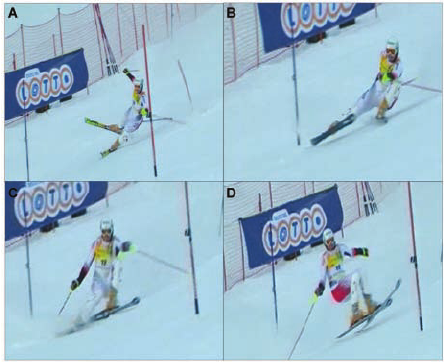
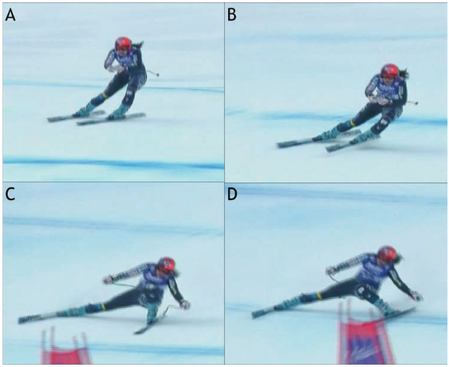
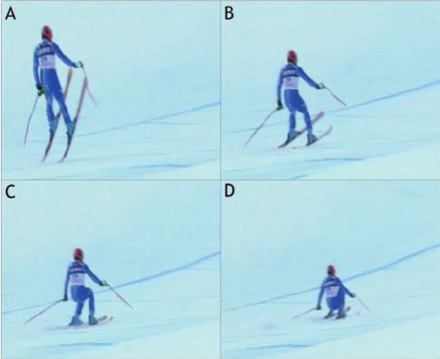
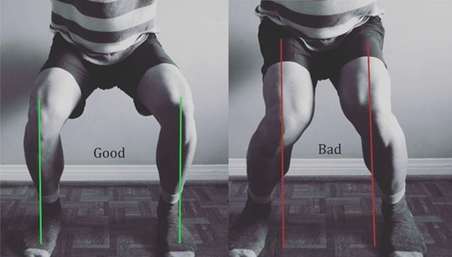
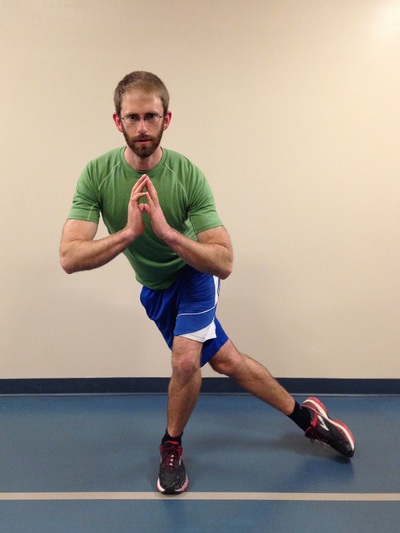
Chances are that if you fall into group 3, you will likely ski and have an injury-free season (but unfortunately there is always a first time for everything…). If you fall into group 1 or 2, you’ll likely appreciate the remainder of the article. Knowledge is power – use the following information to shape your training and awareness! Mechanism of Ski Injuries Fact The knee has two joints – the tibiofemoral joint and the patellofemoral joint. Skiing loads both joints tremendously, in different ways. The two most common knee injuries from skiing include ACL (anterior cruciate ligament) tears, and patellofemoral dysfunction (knee cap pain). ACL Tears ACL tears are acute, and often a result of catching an edge, crashes or poor landings. They often fall into one of three categories: 1) Slip Catch: Commonly seen while turning when the inside edge of the outer ski catches the snow surface, forcing the knee into a valgus collapse and internal rotation position (2). 2) Dynamic Snow Plow: When one of the ski edges accidentally engages the inside edge of the skis, and forces the lower leg to jerk inwards (valgus collapse). The tibia rapidly moves across the middle of the body and cause the valgus collapse of the knee. (1). 3) Landing Back-Weighted: A tactical error in jumping / landing and technique that leads to landing on the tails of the ski, which will stress the knee joint in an anterior/posterior shearing nature (1). Patellofemoral Pain Patellofemoral pain often comes on from an accumulation of poor or excessive loading. The most common fault (and easiest to identify) is a valgus collapse of the knee. You can also identify this by watching someone squat or lunge, or squat / jump, as seen below. If the knee has a tendency to collapse inwards, the hip is usually doing a poor job stabilizing the knee. Other possible reasons for patellofemoral pain include overuse of the quads (anterior chain dominance, too much skiing too soon), tight quads (causing compression of the patella) or weak quads (causing poor stabilization of the knee cap for the load being placed). Training for Healthy Knees and an Injury-Free Ski Season An entire training program for proper knee function is outside of the scope of this article, however a couple good examples include:
General loading principles to abide by include:
A reasonable list of exercises (from basic to advanced) include: Two Leg Focused Exercises Hopping (forward/backwards, side to side, diagonals) Squat Jumps Burpees (with jump) Box Jumps Lateral Box Jump Overs (side to side) Hurdle Bounds Single Leg Focused Exercises Ski Hops Jumping Lunge Single Leg Hopping (forward/backwards, side to side, diagonals) Single Leg Hopping (through cones or agility ladder) Single Leg Hurdle Bounds Perfecting Your Technique During the early part of the ski season, spend the first few ski days working on your technique. Perhaps some pointers from your friends or a ski instructor would be helpful? As you scroll up and review the possible injury mechanisms, remember that strength and, more importantly, technique are to blame for most ski injuries. Pre-Season Stoke Now is the time to make a game plan. If you are excited for ski season, let this fuel your training! Any level of commitment to pre-season strengthening is better than nothing! The ideal goal would be to get into the gym 3 times a week for strength training, but start with whatever you can commit to. If you currently have pain, and aren't sure where to start, make an appointment with a physiotherapist or sports medicine physician. See you out there! References 1) Bere, T., Flørenes, T. W., Krosshaug, T., Nordsletten, L., & Bahr, R. (2011). Events leading to anterior cruciate ligament injury in World Cup Alpine Skiing: a systematic video analysis of 20 cases. Br J Sports Med, bjsports-2011.
2) Bere, T., Mok, K. M., Koga, H., Krosshaug, T., Nordsletten, L., & Bahr, R. (2013). Kinematics of anterior cruciate ligament ruptures in World Cup alpine skiing: 2 case reports of the slip-catch mechanism. The American journal of sports medicine, 41(5), 1067-1073.
1 Comment
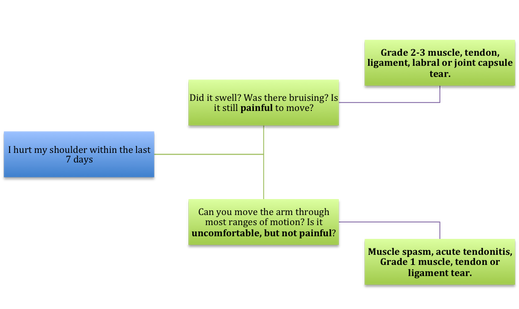
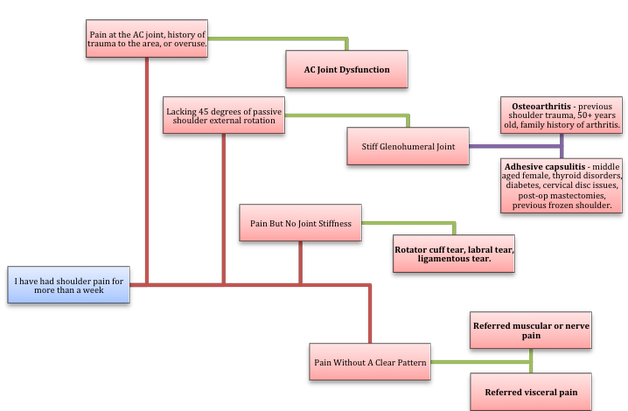
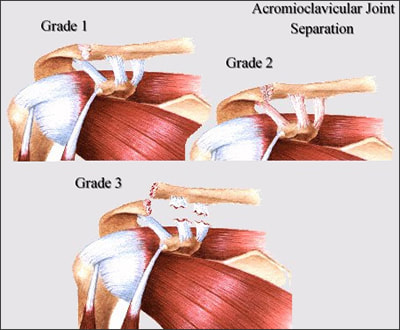
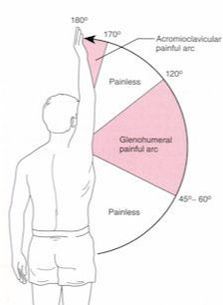
If Only Our Bodies Came With User Manuals! It's tough to know when its okay to push through pain or stiffness, or to know if the recent shoulder tweak that happened last week is of any importance. Over the last number of years I've picked up a number of strategies from research and experts in the sports medicine and orthopaedic world - I hope this can serve as a general guide! (NB - this is a blue print for simple shoulder injuries, and will not fit every situation. Use the following information as the guide that it is, and seek additional advice if you need further guidance!) Did You Hurt Your Shoulder Within The Last 7 Days? To start it off, if you've hurt your shoulder in the last 7 days, read through the following flow chart, and then the corresponding text below: Grade 2-3 muscle, tendon, ligament, labral or joint capsule tear If you experience significant pain, possibly with swelling or bruising, it is likely that you have significantly injured your soft tissues. While outliers exist (bone fracture or nerve involvement), it is most likely an issue related to a tear of a muscle, tendon, ligament, or the joint structure, If the pain in significant, a trip to the ER or family doctor may be the best first option. In terms of rehabilitation, it is probably best to let the shoulder heal for at least 7 days from the initial injury date before starting active rehab exercises. During this time you should see your local physiotherapist or sports medicine physician for an accurate diagnosis and to develop a treatment plan. During the first 7 days, you can support the shoulder with tape or a sling, apply ice (if you need to numb the pain), and perform pain-free range of motion. You should continue to exercise your lower body during this time. You can reasonably expect that there will be a range of motion limitation and/or strength reduction for at least 3 weeks from the date of the injury. It would be advisable to avoid loading the injured tissues with exercise for at least 3 weeks as the injury heals. As per standard tissue healing timelines, the injured tissues will not reach their full strength for up to 9-12 months in a healthy adult… so it is important that you do not re-injure it in the first 3-6 months (to be conservative). Muscle spasm, acute tendonitis, grade 1 muscle, tendon or ligament tear. If you've come to the conclusion that it's likely a muscle spasm, or minor muscle strain / ligament sprain, start immediately with soft tissue release, foam rolling, and gentle stretching into the areas of tightness. Within the first 3-7 days, start to do some light and pain-free resistance exercises to the surrounding muscles (e.g. easy rotator cuff exercises with a theraband). By the end of week 2 you should have loosened up most of the muscle tightness around the shoulder, and should be starting to gradually increase load/exercise for the shoulder. If your discomfort and limited range of motion is not gone within the first 2 weeks, get it assessed and treated. These small nagging injuries have a way of accumulating over the years and may predispose you to a more severe problem in the future. Have You Had Shoulder Pain For More Than 7 Days? This becomes more complicated as we have to discern between a number of different potential concerns. Acromioclavicular (AC) joint dysfunction - There are a few differed reasons that you may develop AC joint dysfunction. First, and most simple, is a direct hit to your shoulder. You will remember this happening, so in this case, its not too complicated. You will likely experience pain and joint laxity when you press on the AC joint, and in severe cases you may experience a 'separated shoulder' that looks like this: The good news about separated shoulders is that physiotherapy (as opposed to surgery) is often enough to help athletes and recreationalists return to their sports and daily activities pain free. If you do not remember a direct trauma, the following may apply to you: The AC joint is often the site of arthritis and come on from overuse or impact (most often seen in athletes (hockey, football, baseball, weight lifters, or overhead work). Pain and dysfunction from the AC joint often can cause impingement of the rotator cuff, and as such may present with muscle weakness, pain down the arm as far as the elbow, and a painful arc of motion. The symptoms that you experience during the arc of motion can help differentiate if it is just the joint that is irritable, or if there may be a rotator cuff impingement; If you have pain between 45-120 degrees abduction, but no pain before or after this range, then it is likely that you have an impingement of supraspinatus muscle (with or without an inflamed bursa). If you only have pain at the very top of this range of motion, it is likely that your AC joint is irritable. Assessment-informed treatment is often the key if it is a chronic pain: 1) You may benefit from other tests that can be done by a physiotherapist to assess joint integrity. 2) An X-ray may be of benefit to ensure there is no bone spur or congenital abnormality of the acromion, 3) A diagnostic ultrasound may be helpful to discern whether the supraspinatus tendon or subacromial bursa are irritated. Conservative treatment is the first-line treatment, as you will almost certainly have tightness and weakness of the surrounding shoulder musculature which may be causing secondary pain. A good assessment is usually needed to assess and treat the neck, thoracic spine, scapulothoracic rhythm, sternoclavicular joint mobility, scapulohumeral rhythm, and the AC joint. Most importantly, returning to a quality, pain-free exercise program will quicken the recovery. Differentiating Reasons for a Stiff Shoulder JointOne of the easiest ways to assess a stiff joint, is to look at passive range of motion, and try to assess the end-feel of the motion. If you are lacking 45 degrees of passive shoulder external rotation, and it feels like there is a capsular or joint restriction (hard end-feel), you likely fit into this category. Often, these cases require a medical approach to rule out other pathologies - be prepared to seek a referral to your family doctor or sports medicine physician for some imaging (to rule out sinister pathology or rule in arthritis), or blood work.  To assess passive shoulder external rotation, lay down on your back, and with you painful arm completely relaxed, use a broomstick or cane to gentle push the painful arm outwards (rotating the shoulder out). Keep your elbow relaxed and next to your ribcage. Remember... you are trying to assess the stiffness of the joint, so all muscles in the painful arm must remain relaxed! Glenohumeral Osteoarthritis If you have had a previous shoulder trauma, are 50+ years old or have a family history of arthritis, the most likely problem is that of glenohumeral osteoarthritis (could be from previous instability, or because of normal wear and tear associated with age). Manual therapy that focuses on improving joint capsule mobility is often required to make progress. Various joint injections exist that may help with lubrication of the joint, or inflammation within the joint. At home, patients can start with rolling tight muscles on the back of the shoulder joint to loosen any tissues that may be restricting the joint mobility. Ultimately, most progress will be made with the help of physiotherapy or medical intervention. Adhesive Capsulitis (Frozen Shoulder) The most likely alternative reason for a stiff shoulder is adhesive capsulitis. The strongest risk factor for developing adhesive capsulitis is being a peri-menopausal female. Other risk factors include thyroid disorders, diabetes, cervical disc issues, post-op mastectomies, a recent fall/trauma, and having a previous frozen shoulder. The shoulder seems to stiffen and become painful without a usual cause, and keeps patients awake at night. We see patterns of limited external rotation, internal rotation and flexion. If the diagnosis of adhesive capsulitis is reached, patients may find a cortisone injection helpful in the early stages. There has also been some clinical evidence showing that manipulation of the fibrotic joint under a nerve block may be of benefit.. Otherwise, regular physiotherapy that includes stretching, shockwave therapy, and manual therapy (soft tissue release, IMS, and joint mobilizations) will provide the greatest benefit. Shoulder Pain with Limited Active Range of Motion but Without Joint Stiffness If you do not have a stiff glenohumeral joint (more than 45 degrees passive external rotation), yet there is shoulder pain and limited active range of motion, a skilled practitioner will take you through a number of tests to help determine whether the pain is coming from a rotator cuff tear, labral tear or ligamentous tear (this is usually preceded by a dislocation / subluxation). The diagnosis of a tear must be ascertained by the clinic history, movement exam, special tests, response to treatment, and possibly ultrasound/MRI/other imaging. For the purposes of this article I am going to avoid the discussion of which special tests may be useful for diagnosing tears; This is a contentious issue as most special tests are... not that special; they are not very specific toward testing just one tissue and often lead to false positives. This topic is beyond the scope of this article. Shoulder Pain Without a Clear Pattern Very few patients fit into this category, so if you think that you do, its likely that you've missed something during your self-assessment. Excluding this caveat, I write this last section for completion. 1. Referred Pain - A painful shoulder that has no pattern of painful movement may be experiencing referred symptoms from the neck, diaphragm or the heart. 2. Cancer/Metastases - A number of different viscera can create pain into the shoulder region. Most likely include the lung, liver, and gallbladder. Typically you will experience unrelenting pain (nothing can make the symptoms change), difficulty sleeping at night, excessive fatigue, weight loss, a fever, or any number of other changes in your normal health. See the following link for more information: https://www.cancer.org/cancer/cancer-basics/signs-and-symptoms-of-cancer.html 3. Pain Syndromes - Widespread hypersensitivity/hyperalgesia may also affect the shoulder. Various non-specific pain syndromes may create shoulder pain and include: Chronic Regional Pain Syndrome, Myofascial Pain Syndrome & Fibromyalgia. A Final Note In most cases of shoulder pain, an exercise program is the key component necessary to return to full function without pain. In cases of partial thicken tendon tears, full thickness tendon tears or subacromial impingement, a specific and progressive exercise program often provides improved function, reduced pain and reduced need of surgery when compared with a general exercise program (1, 2, 3). My typical progression in the clinic is: 1) Determine if patient has any red flags that indicate immediate medical assessment / intervention. 2) Assess full body movement to determine how one area of the body may be affecting another. 3) Assess the shoulder for joint integrity, ligament and tendon damage, flexibility and strength. 4) Perform manual therapy, IMS and shockwave (if needed) to reduce pain and improve joint position/posture. 5) Provide patient with a specific, graduated exercise program. 6) Assess progress of the shoulder and repeat 2-6 as indicated until full function is .recovered, or a referral is indicated to see a sports medicine specialist. References (1) Björnsson Hallgren, H. C., Adolfsson, L. E., Johansson, K., Öberg, B., Peterson, A., & Holmgren, T. M. (2017). Specific exercises for subacromial pain: Good results maintained for 5 years. Acta Orthopaedica, 1-6.
(2) Holmgren, T., Hallgren, H. B., Öberg, B., Adolfsson, L., & Johansson, K. (2012). Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study. Bmj, 344, e787. (3) Kukkonen, J., Joukainen, A., Lehtinen, J., Mattila, K. T., Tuominen, E. K. J., Kauko, T., & Äärimaa, V. (2014). Treatment of non-traumatic rotator cuff tears. Bone Joint J, 96(1), 75-81. Consistent Training Leads to Skilled Running Most athletes will attest that consistency is the most important aspect in progressing fitness and skill through training. This is why injuries set you back from reaching your full potential, or at least reaching goals in a timely fashion. While running, there are many things we can do to prevent injuries and some of them require very little time to implement, although learning the most effective way to implement them is individualized and may take years to achieve personal efficiency. Indeed, running is a skill, and it takes a long time to learn how to use your body in the most effective way. With a good training plan you will improve your efficiency, which will reduce physical and mental fatigue, reduce injury risk, and ultimately improve your performance! If you are new to running, or are simply wanting to improve, try these movement tweaks the next time you head out the door. N.B . These tweaks are good guidelines, but if you have a preexisting dysfunction (remember a dysfunction may not present with pain or any other symptom), you may benefit from a personalized approach. If you fall into this group, book in for a running assessment or seek guidance from a running coach, or rehab professional with post-graduate training in running assessments. It's Much More Than One Foot in Front of The Other 1) Upright posture. "Be tall!" At the start of your run, and periodically during your run, remind yourself to be tall. Think about elongating your entire spinal column; That is... if you had a string attached to the top of your head that connects down through the middle of your body, think about pulling that string up! You should not dramatically change your spinal curve with this, but you should feel that you are slightly taller. Why? When done appropriately, this helps to engage your multifidus muscles (spinal stabilizers), and make you aware of your core. This will help prevent energy loss due to poor stability, and will better allow you to apply force through your hips - helping to propel you forwards. It also helps with diaphragmatic activation and reduces the amount of airway resistance during breathing. PS - it might be a good idea to start thinking about upright posture during the rest of your day, as we spend thousands of hours hunched over at work and at home each year, and BELIEVE IT OR NOT!, this affects our athletic performance! 2) Forward lean from the feet / ankles "Lean forward from the ankles!" Running should be efficient. Leaning forward from the ankles aids in this efficiency, because it moves your center of mass slightly forward, and allows you to fall into your next stride. Don't forget #1 - it is too easy to let your forward lean come from hinging at the hips - "Stay Tall", and keep your head up, as you need to be looking forward! 3) Posterior-chain propulsion "Push, don't pull!" If we lean forward from the ankles, we will fall forward and must flex our hip joint and extend our knee to "catch" us from falling on our face. We can use this forward energy most effectively by pushing ourselves forward, as soon as our foot hits the ground. Try to see if you can feel yourself pushing forward using your glutes, hamstrings and calves. 4) Shortened stride and increased cadence "Shorten your stride and increase your cadence!" "Imagine that you are a ball, and as you are rolling over the ground, you are attempting to touch as many different places on the ground as possible" Most research suggests that elite runners who stay injury-free run with a cadence between 160-190 BPM. In most runners this improves multiple metrics (decreased "breaking phase", decreased vertical oscillation, decreased need for force absorption), and ultimately it decreases the amount of wear and tear / abuse placed on joints and muscles. In addition, it is said to improve efficiency in the long-term after the athlete adjusts to running in this way. The best place for our foot to land is directly under our center of mass because it minimizes the "breaking phase". The breaking phase is best described as wasted energy in the time between the foot striking the ground, and the push off phase when we propel ourself forwards. To ensure that we land with a vertical tibia - it is crucial to having a high cadence and a shortened stride. 5) Land with your foot under your center of mass "Most often, you should land using a midfoot strike" The jury is still out on what the best type of foot strike looks like in endurance athletes, but here is what we do know: A) A midfoot strike is mostly likely to place the foot under your center of mass while running on flat ground. B) Landing with a forefoot strike lends to a 2.6 times decrease in injury risk compared to rearfoot strikers (1). C) Landing on the forefoot or midfoot places more stress on the foot musculature and Achilles tendon. Landing on the rearfoot places more compressive loading forces at the tibiofemoral and patellofemoral joints of the knee. C) Rearfoot strikers tend to land with their foot in front of the body, which leads to have a longer stride and greater vertical loading (increased forces applied to the body) (2). D) Wearing shoes with larger heels lends to heel striking, whereas taking shoes off leads to landing on the forefoot or midfoot, with the strike being closer to the body. As always, we are reminded that science has limitations and common sense prevails, therefore do what feels right... BUT my recommendation would be to run on variable terrain, AND: A) As you run uphill, strike with your forefoot or midfoot. B) As you run the flats, strike mostly with your midfoot. C) As you run downhill, midfoot or heel strike may be best. Concluding Remarks These are but a few ways to immediately change your running form, in an effort to improve efficiency and promote injury-free training. General recommendations are terrible because they assume that all people are alike, so make no mistake - it is probably best to have a running assessment done to determine whether you truly need to change your running form. Nevertheless, exposing yourself to learn different styles of running will grow your running skill-sets and your body's durability, ultimately making you a better athlete! References 1) Daoud, Adam I., et al. "Foot strike and injury rates in endurance runners: a retrospective study." Med Sci Sports Exerc 44.7 (2012): 1325-34.
2) Williams III, Dorsey S., Irene S. McClay, and Kurt T. Manal. "Lower extremity mechanics in runners with a converted forefoot strike pattern." Journal of Applied Biomechanics 16.2 (2000): 210-218. IntroductionThis article is meant to provide education to current clients, future clients, or any other interested parties. It will provide a basic level of knowledge which is available in the current research and should help to answer your question including: "How does it work?", and "Why does my muscle twitch when you put a needle there?!" Intramuscular Stimulation (IMS) is one of the most effective techniques available to reduce muscular pain and tightness; Essentially IMS 'resets' trigger points (TrPs) to allow for normal muscle contraction and relaxation. The technique is known by many names: IMS, GunnIMS, Dry Needling, Functional Dry Needling (FDN), Trigger Point Needling, and Intramuscular Manual Therapy. Regardless of the name, all methods use the same theory and should attain similar results, providing the diagnosis is correct and the practitioner is competent. The most recent systematic review, published in 2015, analyzed 25 high-quality studies and found significant improvement in pain, range of motion, function and quality of life when IMS was used in multiple body regions (1). Its reputation has become well-known: Many advocates from the medical and research community call IMS the most important contribution to pain science and treatment in the last 20 years. As a result it has become a highly sought after skill-set in professional sport, chronic pain centers and physiotherapy clinics everywhere. TrPs have been scientifically acknowledged since the early 1900s, when Sir William Gowers introduced the (now dated) term “fibrositis”, meaning a palpable tenderness and hardness of a muscle. Significant headway was made in the 1970s by Dr. Janet Travell (MD for Presidents Kennedy and Johnson) who authored research documenting TrP pain referral patterns. However, it wasn’t until Dr. Chan Gunn introduced his theories and supporting research in the late 1990s that IMS started to gain formal recognition as a treatment modality. Physiotherapists and physicians with specialized post-graduate training perform IMS. A thorough physical examination proves indispensable as chronic pain is neurologically driven (as opposed to structural), and therefore it is undetectable by X-rays, MRI Tests, Bone and CT Scans. If relevant TrPs are found on examination, a sterile acupuncture needle is then inserted and moved for 1-5 seconds in the tight muscle, causing a cramping or twitch response of the muscle. Needles may also be inserted near the spine where nerve roots have become irritated and hypersensitive. Before we can examine the effects of IMS on TrPs, let's first identify what we know about them. Three Types of Trigger Points There are three types of trigger points: Active Trigger Points – A hyperirritable spot in a taut band of skeletal muscle/fascia which is painful without being touched (but more painful with compression) and produces characteristic pain, referred symptoms, motor dysfunction and/or autonomic nervous system signs/symptoms. Latent Trigger Points – A hyperirritable spot that is painful with compression, but does not have referral symptoms. Satellite Trigger Points – A latent point that develops in a synergist muscle, antagonist muscle, muscle with common neural link or the same pain referral zone. These trigger points may become symptomatic neurogenically or mechanically by an increased irritability of the key TrP. Trigger Point Characteristics Trigger points have been studied thoroughly in the research. Here is what we know to date:
B) Elevated neurotransmitters and neuropeptides involved in pain sensitivity, vasoconstriction, vascular permeability, mast cell degranulation (mast cells release inflammatory components), increased sympathetic activity in motor endplate regions of TrP, decreased feedback control of muscle length and increased spontaneous electrical activity at motor endplates (14). C) Elevated cytokines and chemokines involved in inflammation, immune regulation, sensitivity of nociceptors and increased pain in the muscle (14). Physiological Effects of IMS As we insert an acupuncture needle into a TrP, a reset of the neuromuscular system occurs. This results in reduced local and referred pain (15, 16), improved range of motion (2, 3) and decreased TrP irritability both locally (7, 17) and remotely (8, 18). It is also proposed that these changes reduce associated dysfunction caused by the pulling effects of the tight muscles across joints, discs, nerves, tendons, etc. These results occur for the following reasons:
Conclusion IMS requires a medical examination and diagnosis by a practitioner knowledgeable in musculoskeletal pathology and human anatomy. The technique is supported by high-quality research, and when applied correctly, it can help provide lasting relief to patients with acute and chronic pain. References1) Boyles R, Fowler R, Ramsey D, Burrows E. Effectiveness of trigger point dry needling for multiple body regions: a systematic review. Journal of Manual and Manipulative Therapy. 2015 Jun 18:2042618615Y-0000000014.
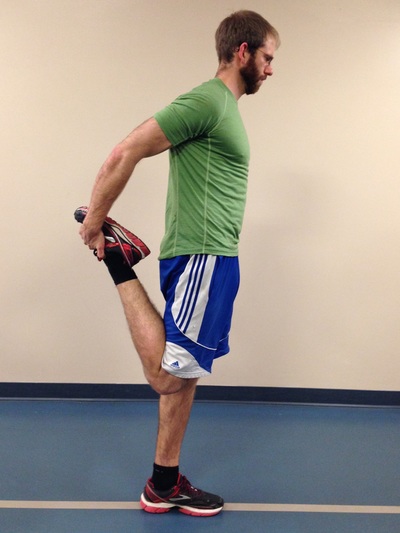
2) Lucas KR, Rich PA, Polus BI. Muscle activation patterns in the scapular positioning muscles during loaded scapular plane elevation: the effects of latent myofascial trigger points. Clin Biomechanics. 2010;25(8):765-770. 3) Lucas KR, Polus BI, Rich PS. Latent myofascial trigger points: their effects on muscle activation and movement efficiency. J Bodyw Mov Ther. 2004;8:160-166. 4) Ballyns JJ, Shah JP, Hammond J, Gebreab T, Gerber LH, Sikdar S. Objective sonographic measures for characterizing myofascial trigger points associated with cervical pain. J Ultrasound Med. Oct 2011;30(10):1331-1340. 5) Brückle W, Sückfull M, Fleckenstein W, Weiss C, Müller W. Gewebe-pO2-Messung in der verspannten Rückenmuskulatur (m. erector spinae). Z. Rheumatol. 1990;49:208-216. 6) Ge HY, Fernandez-de-Las-Penas C, Yue SW. Myofascial trigger points: spontaneous electrical activity and its consequences for pain induction and propagation. Chin Med. 2011 Mar 25;6(13):1-7. 7) Kuan TS, Hsieh YL, Chen SM, Chen JT, Yen WC, Hong CZ. The myofascial trigger point region: correlation between the degree of irritability and the prevalence of endplate noise. Am J Phys Med Rehabil. 2007;86(3):183-189. 8) Hsieh YL, Chou LW, Joe YS, Hong CZ. Spinal cord mechanism involving the remote effects of dry needling on the irritability of myofascial trigger spots in rabbit skeletal muscle. Arch Phys Med Rehabil. Jul 2011;92(7): 1098-1105. 9) Rha DW, Shin JC, Kim YK, Jung JH, Kim YU, Lee SC. Detecting local twitch responses of myofascial trigger points in the lower-back muscles using ultrasonography. Archives of physical medicine and rehabilitation. 2011 Oct 31;92(10):1576-80. 10) Chen Q, Bensamoun S, Basford JR, Thompson JM, An KN. Identification and quantification of myofascial taut bands with magnetic resonance elastography. Archives of physical medicine and rehabilitation. 2007 Dec 31;88(12):1658-61. 11) Shah JP, Danoff JV, Desai MJ, et al. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil. Jan 2008;89(1):16-23. 12) Shah JP, Gilliams EA. Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: an application of muscle pain concepts to myofascial pain syndrome. J Bodyw Mov Ther. Oct 2008;12(4):371-384. 13) Shah J, Phillips T, Danoff JV, Gerber LH. A novel microanalytical technique for assaying soft tissue demonstrates significant quantitative biomechanical differences in 3 clinically distinct groups: normal, latent and active. Arch Phys Med Rehabil. 2003;84:A4. 14) Shah JP, Phillips TM, Danoff JV, Gerber LH. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. Journal of applied physiology. 2005 Nov 1;99(5):1977-84. 15) Affaitati G, Costantini R, Fabrizio A, Lapenna D, Tafuri E, Giamberardino MA. Effects of treatment of peripheral pain generators in fibromyalgia patients. Eur J Pain. Jan 2011;15(1): 61-69. 16) Srbely JZ, Dickey JP, Lee D, Lowerison M. Dry needle stimulation of myofascial trigger points evokes segmental anti-nociceptive effects. J Rehabil Med. 20110;42(5):463-468. 17) Chen JT, Chung KC, Hou CR, Kuan TS, Chen SM, Hong CZ. Inhibitory effect of dry needling on the spontaneous electrical activity recorded from myofascial trigger spots of rabbit skeletal muscle. Am J Phys Med Rehabil. Oct 2001;80(10):729-735. 18)Tsai C-T, Hsieh L-F, Kuan T-S, Kao M-J, Chou L-W, Hong C-Z. Remote effects of dry needling on the irritability of the myofascial trigger point in the upper trapezius muscle. Am J Phys Med Rehabil. 2010;89(2):133-140. 19) Cagnie B, Barbe T, De Ridder E, Van Oosterwijck J, Cools A, Danneels L. The influence of dry needling of the trapezius muscle on muscle blood flow and oxygenation. Journal of manipulative and physiological therapeutics. 2012 Dec 31;35(9):685-91. 20) Hsieh YL, Yang SA, Yang CC, Chou LW. Dry needling at myofascial trigger spots of rabbit skeletal muscles modulates the biochemicals associated with pain, inflammation, and hypoxia. Evidence-based complementary and alternative medicine. 2012 Dec 23;2012. 21) Niddam DM, Chan RC, Lee SH, Yeh TC, Hsieh JC. Central modulation of pain evoked from myofascial trigger point. The Clinical journal of pain. 2007 Jun 1;23(5):440-8. The Great Outdoors. It is there for you to enjoy, to push your limits, and develop fortitude. For some people, going outdoors can be synonymous with developing injuries, but there are steps you can take to mitigate future injuries from taking place. The Right Fitness Level Greater fitness leads to a better understanding of your limits, as well as the ability to achieve greater feats. A physical assessment by a good therapist or strength and conditioning coach can help you sort through the thousands of exercises out there to know which ones are relevant to your needs. - Slow, gradual increases in exercise and specific training are necessary (months and/or years). Our bodies adapt well to gradual stresses, but if too much load is placed on it at once, expect failure and injuries. It takes great dedication to yield great results. Most outdoor athletes peak in their 30s and 40s as they build cardiovascular endurance, muscular endurance, and a resistance to injury. - Outdoor athletes often suffer overuse / over-training. It is important to consider whether you have proper body mechanics during training and outdoor pursuits. Have knowledgeable therapists, coaches and other athletes watch your form and provide suggestions. It is also important to include adequate cross-training, regular body maintenance (physiotherapy, massage, rolling), proper nutrition, and adequate rest. - As a general rule there are certain joints which must be stable (strong ligamentous and muscular support around the joint, which prevents excess joint motion) and others which must have good mobility (the joint is built to be very flexible, however the muscular support around the joint must be able to control this increased range). As pertaining to lower body exercise, the core must be stable, hips must be mobile, knees must be stable, and the ankles must be mobile (Cook, Burton & Kiesel, 2010). Try adding the following 20-minute routine into your regular workouts, three days a week. It is a small corrective exercise program built to help the user become more aware of hip / knee / ankle positioning during single leg stance. It is not meant to replace regular strength training. Rather, it should enforce the principles of joint alignment, feeling posterior chain engagement and will allow good transfer to outdoor pursuits. A) Dynamic stretching. Perform dynamic stretching prior to exercise for 30 seconds per muscle group. A few lower body ideas include front/back and side-to-side leg swings, quick quadriceps stretches, quick piriformis/glute stretches, and hopping. B) Airplane. At first you may need to hold onto something for balance, but eventually you should be able to progress to no hands. Goal = 10 reps per side. C) Step-ups. Face a mirror and line up the hips and knees on the working leg to be approximately 90 degrees. Ensure that during the exercise, your knee tracks straight (not allowing it to collapse inwards or outwards). Lean forward, try to feel your glutes and hamstring fire on the upper leg then push through the heel on the working leg as you step up (this will help you to activate the posterior chain). Goal = 10 reps per side, with 2 times the expected weight of your backpack and gear. D) Single leg star balance. Reach as far in each of the four directions as possible, while bending the stance leg at the hip and knee during the reaching phase (this leg should remain straight in line from the hip to the foot). Goal = 10 reps for each leg. 1 rep = a full cycle of the four directions. Side note: Work to create symmetry in this test, as evidence suggests that a difference of more than 4 cm between left and right legs in ‘the forward reach’ component can help predict whether an athlete is at risk of injuring the leg (Smith, Chimera & Warren, 2014). Tip: Place masking tape on the ground and mark the distance in centimeters. E) Piriformis rolling and pigeon stretch. 1 minute rolling, 1 minute stretch per side. F) Lateral Quadriceps rolling and stretch. 1 minute rolling (focus on the outside of the leg), 1 minute stretch per side.
|
| Start With The Right Intel - Create specific training goals: How many days/hours, what gear do I need to use, am I familiar with the terrain? - Become efficient and effective in your skill-set by learning the best decision making skills and techniques via free resources (friends, books, videos), and progressing to courses or hiring a guide. | The Right Gear - Hiking poles take up to 25% of stress off your knees during descent (Schwameder, et al., 1999) help your legs save energy, and improve your balance on technical terrain. - Boots that fit well can prevent crushed toes, and rolled ankles. - Bring microspikes, mountaineering gear and/or avalanche gear if you expect snowy conditions. |
References
Schwameder, H., Roithner, R., Müller, E., Niessen ,W., Raschner, C. (1999).
Knee joint forces during downhill walking with hiking poles. Journal of Sports Science, 17(12): 969-978.
Smith, C.A., Chimera, N.J., Warren, M. (2014). Association of Y balance test reach asymmetry and injury in division I athletes. Medicine and Science in Sports and Exercise. Epub ahead of print.
Author
Jacob Carter lives and works in Canmore, Alberta. He combines research evidence with clinical expertise to educate other healthcare professionals, athletes, and the general public on a variety of health topics.
Archives
November 2022
July 2022
January 2022
February 2020
May 2019
April 2019
July 2018
May 2018
March 2018
January 2018
October 2017
September 2017
March 2017
February 2017
December 2016
November 2016
October 2016
May 2016
March 2016
January 2016
June 2015
February 2015
December 2014
October 2014
September 2014
Categories
All
Aging Population
Annual Check Up
Annual Check-up
Annual Physiotherapy Assessment
Calgary
Canmore
Climbing
Collaborative Care
Concussion
Core Muscles
Disease Prevention
Exercise
Exercise Selection
FDN
Frozen Shoulder
Functional Dry Needling
Health
Health Promotion
IMS
Inflammation
Injuries
Injury Prevention
Intramuscular Stimulation
Jacob Carter
Literature Review
Lumbar Spine
Manual Therapy
Mountaineering
Pain
Personal Training
Physiotherapy
Preventative Medicine
Rehabilitation
Research
Shoulder Impingement
Shoulder Injuries
Skiing
Ski Injuries
Ski Season
Swelling
Tendinopathy
Tendinosis
Tendon
Tendonitis
Trail Running
Wellness
|
|



















 RSS Feed
RSS Feed